Effectiveness of MRI vs CT in Diagnosing Hepatic Lesions: A Systematic Review
Click here to access top-notch assignment help provided by our native assignment help company.
Introduction: Assessing MRI and CT Diagnostic Accuracy for Liver Abnormalities
1. Background
1.1 Description of hepatic lesions
A liver lesion is considered abnormal growth in the liver, which can be developed for multiple reasons. This lesion can also lead to cancer if an effective therapeutic approach is not infused at the right time. Benign lesions or noncancerous lesions are common in individuals (Cleveland Clinic 2022). On the other hand, liver cancer is another type of hepatic lesion, which can be fatal for individuals. Among benign hepatic lesions, hepatic hemangioma is the most common and it occurs among 5% of adults. Similarly, focal nodular hyperplasia is another type of benign hepatic lesion and occurs among female individuals. Liver cysts are another significant type of benign hepatic lesion (Rawla et al. 2019).
Severe alcoholism or viral hepatitis can develop hepatocellular carcinoma, which eventually develops into metastatic liver cancer. One of the significant ways to diagnose hepatic lesions is the abdominal imaging techniques, such as CT (computed tomography) scan and MRI (magnetic resonance imaging) (Rating 2022).
Thus, hepatic lesions can be divided into two major parts, which are benign liver lesions and liver cancer. Each stage of liver lesions can be differentiated into different stages, which can be characterized by different types of symptoms.
Benign liver lesions
Different types of benign hepatic lesions include the following types,
- Focal nodular hyperplasia:
This is a common benign tumor in the liver, which can be seen frequently in patients. FNH (focal nodular hyperplasia) is a regenerative mass lesion in the hepatic region. This has a unique radiographic feature, which can be seen through multimodality imaging techniques. Besides, some of the lesions can be atypical in appearance (Venturi et al. 2017). Being asymptomatic, no additional treatment is required for this abnormality. Exogenous estrogens do not cause the formation of nodular hyperplasia and do not increase the size of the mass. However, de novo hyperplasia can be seen after chemotherapy treatment with oxaliplatin.

Figure 1: Focal nodular hyperplasia
- Liver hemangioma:
This is a benign mass in the hepatic region made up of a cluster of blood vessels. This disorder is also known as cavernous hemangioma and it can be seen approximately in 20% of the entire population (Eghlimi et al. 2020). It is the most common type of hepatic lesion. This can be detected and diagnosed with the help of imaging techniques.
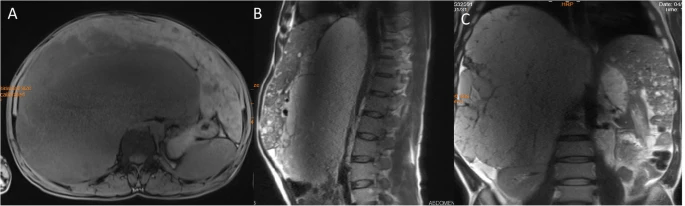
Figure 2: T1-weighted MRI image of liver hemangioma
- Liver cysts:
This type of hepatic lesion is generated due to fluid-filled cavity generation in the liver. Those cavities can grow significantly in terms of generating pressure on the hepatic walls and creating tremendous pain (Allan et al. 2020). Computed tomography (CT) has the upper hand in detecting liver cysts. Liver cysts can generate numerous adverse hepatic abnormalities, such as polycystic liver disease, echinococcus infection, and even hepatic cancer.
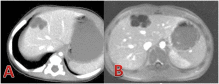
Figure 3: CT scan of liver cysts
- Hepatic adenoma:
Hepatic adenoma is considered a benign hepatic lesion, which is linked with anabolic steroids, as well as oral contraceptive pills. This condition indicates the formation of a benign hepatic tumor (Shreenath and Kahloon 2022). It is generated in hepatocytes and caused by a genetic mutation. Alteration in the level of anabolic steroids is one of the prime reasons for generating this type of hepatic lesion.

Figure 4: CT Image of hepatic adenoma
Liver cancer
Different types of liver cancer can be categorized into the following orders,
- Metastatic hepatic cancer:
Hepatic metastases are a type of liver cancer, which tends to spread to another part of the body from hepatic cells. Most commonly the cancer is spread to the rectum or colon. This type of hepatic lesion showcases tremendous abdominal pain in the upper abdominal area (Kow 2019). Besides, ongoing fatigue can be seen in this type of hepatic lesion.
- Hepatocellular carcinoma:
This is the most common type of primary liver cancer. This type of hepatic lesion can be seen in individuals with chronic liver diseases (McGlynn et al. 2020). The major reason behind the formation of hepatocellular carcinoma is hepatitis B and C infection.
1.2 Effectiveness of CT in hepatic lesions
Hepatic lesions can be identified through CT imaging techniques. Non-enhanced computed tomography (NECT) can help identify hepatic tumors (Gore et al. 2017). Besides, the multidetector-row CT imaging technique has been useful for detecting hepatic lesions. Arterial phase imaging techniques can help identify multiple tumor masses within the liver. With the help of contrast differentiation, CT imaging can detect hepatic lesions (Baron 2022). In the case of portal venous phase imaging, contrasting dye is loaded in the portal vein to detect the hypervascular tumors.
Multidetector-row computed tomography (MDCT) is the primary imaging test for staging and following up malignancies, which tend to originate outside the nervous system. This imaging technique helps diagnose metastatic hepatic cancer or hepatocellular carcinoma. In the regions of hepatic lesions, there is the presence of a straight-line margin with the presence of normal parenchyma (Boyum et al. 2021). An associated budging can be seen in that specific area with hepatic contour, as well as vascular displacement. Differentiation in metastatic disease can be seen with the help of CT imaging techniques. However, absolute attenuation values of CT can showcase unreliability, as fatty infiltration can not generate fat-density lesions. However, dual-energy MDCT is significantly impactful in identifying hepatic lesions with a density of more than 20HU (Gore et al. 2018). Below this range can provide a virtual unenhanced image, which can be a problem factor for diagnosing hepatic lesions. Thus, high-density hepatic lesions can be identified with the help of CT imaging techniques.
In a CT scan, a series of X-ray photographs are combined to generate a detailed picture of the target organ. With the help of a ring-shaped x-ray emitting diode, cross-sectional slices are developed and those slices tend to generate an entire picture of the target organ. In CT scanning, an X-ray tends to produce a narrow and fan-shaped beam in terms of irradiating a particular section of the patient's body. The thickness of the fan can be as small as 1 millimeter and can be extended up to 10 millimeters. In CT imaging techniques, there are multiple phases, which are made up of 10-50 rotations of X-ray tubes around the patient (US Food and Drug Administration 2020). Images can be formed in terms of differentiating soft and hard tissues in a particular organ. X-rays tend to penetrate soft tissues and a detailed overview of hepatic lesions can be generated with the help of CT imaging techniques.
1.3 Effectiveness of MRI in hepatic lesions
In terms of determining hepatic masses, magnetic resonance imaging (MRI) is the most effective imaging technique. With the help of "high intrinsic soft-tissue contrast", a high-quality image of hepatic lesions can be generated (Albiin 2022). Automated contrast-detection methods can be combined with faster sequences and this approach can capture images of arterial phases. Thus, hepatic lesions can be characterized and differentiated. With the help of T1 and T2-weighted sequences, liver lesions can be diagnosed. Diffusion-weighted imaging techniques can help detect hepatic lesions through contrast generation between soft tissues (Gangahdar et al. 2018).
Magnetic resonance imaging (MRI) technology is the most sensitive, as well as a specific imaging technique for the characterization and detection of hepatic masses, which also include metastases. In the case of sensitivity, positive predictive value, and specificity, MRI can detect hepatic lesions more accurately and can differentiate those as per their classes. Malignant hepatic lesions tend to demonstrate a specific impeded diffusion, which is considered as "high residual signal intensity" on the images, which contain a high b value (Gore et al. 2018). Apparent diffusion coefficient (ADC) values for malignant hepatic lesions are considered to be visually lower than liver parenchyma. Thus, MRI is an effective imaging technique for detecting and diagnosing hepatic lesions accurately. MRI tends to generate contrast-induced images of hepatic lesions for detecting hepatic lesions (Wang et al. 2018). Confirmatory stating MRI can be used significantly for diagnosing hepatic lesions (Rantala et al. 2020).
Magnetic resonance imaging (MRI) technology tends to employ powerful magnetic fields for capturing detailed images of a specific organ. The strong magnetic field forces protons in a particular alignment to create a clear image. When radiofrequency current is pulsed through an organ, the protons are stimulated spin out of equilibrium, and are set against the magnetic pull. Thus, MRI sensors tend to generate an image based on the released protons (National Institute of Biomedical Imaging and Bioengineering 2018). When the radiofrequency field is turned off, the sensors can detect those proton misalignments. In this way, a contract-dependent image is formed, which can help diagnose hepatic lesions.
1.4 Comparison between MRI and CT in hepatic lesions detection
Between computed tomography (CT) imaging and magnetic resonance imaging (MRI), the second one is the most effective imaging technique for diagnosing hepatic lesions. With the help of T1 and T2-weighted sequences, MRI can generate contrast between soft tissues, which tends to indicate hepatic lesions (Wang et al. 2018). On the other hand, with the help of X-rays, CT scans can capture images of hepatic lesions. However, non-enhanced CT scans can not indicate hepatic tumors due to the inherent contrast between tumor tissue and surrounding hepatic parenchyma (Baron 2022).
MRI is considered the most specific and sensitive imaging technique for detecting and characterizing hepatic lesions, including metastases. Positive predictive value and sensitivity can be differentiated in MRI in a specific manner. On the other hand, MRI has some restrictions for usage. Patients with pacemakers cannot use MRI as this imaging technique uses magnetic fields, which can hamper the normal working pattern of pacemakers. On the other hand, an MRI is quite expensive compared to a CT scan (Gore et al. 2018). Malignant masses in the hepatic region can be easily identified with the help of MRI, as impeded diffusion can be seen in this type of hepatic lesion. Thus, high b values can be obtained by MRI, which can differentiate hepatic lesions from surrounding liver parenchyma. On the other hand, the CT imaging technique has been well-accepted in terms of staging a wide variety of malignancies (An et al. 2019). In terms of infused CT scans, it is less sensitive than the contrast-enhanced MRI for characterizing even tiny hepatic metastases with a diameter of less than 1 cm. "Ethoxybenzyl diethylenetriaminepentaacetic acid (EOB-DTPA)-enhanced MRI" showcases superiority in determining hepatic lesions compared to a CT scan (Wang et al. 2018). MRI has the superiority for demonstrating and differentiating hepatic lesions better than CT scans. In CT scans, fat tissues tend to interrupt the proper differentiation of hepatic lesions. On the other hand, MRI is highly insensitive to liver fat infiltration, which results in a sharp image formation of hepatic lobules and can help differentiate hepatic lesions more accurately (Min et al. 2020).
1.5 Research question and justification
Research question: What is the effectiveness of MRI in hepatic lesions diagnosis compared to CT imaging technique?
|
Population (P) |
Intervention (I) |
Control (C) |
Outcome (O) |
|
Patients with hepatic lesions |
CT imaging, MRI |
Use of X-ray imaging technique and magnetic field to determine the level and category of hepatic lesions in patients |
Detection of hepatic lesions and determining the degree through imaging techniques |
Table 1: PICO framework
This research question will help channel this systematic review properly in terms of evaluating the effectiveness of CT and MRI for diagnosing hepatic lesions. Focusing on the PICO-framed question, a concluding statement can be generated focusing on the evaluation of a more prominent imaging technique for diagnosing hepatic lesions. In all the considered journals and articles, patients with different degrees of hepatic lesions have been considered and those individuals have been exposed to both CT and MRI for diagnosing hepatic lesions and differentiating their levels.
2. Search strategy
2.1 Keyword search based on Boolean operator
|
Keywords |
And |
Or |
Not |
|
Hepatic lesions |
Hepatocellular carcinoma, liver hemangioma, nodular hyperplasia, liver cysts |
Liver lesions |
Liver cirrhosis, fatty liver |
|
CT |
Non-enhanced computed tomography, multidetector-row CT |
Computed tomography |
X-ray imaging |
|
MRI |
T1 and T2-weighted imaging |
Magnetic resonance imaging |
Biopsy |
Table 2: Boolean operator table
The boolean operator approach has been utilized in this systematic review for gathering pre-existing journals and articles in scientific databases. With the help of the keywords mentioned above, relevant journals and articles have been considered to analyze the effectiveness of CT imaging and MRI for diagnosing hepatic lesions. Keywords appropriate to the topic of systematic review have been utilized for searching academic journals. However, irrelevant keywords have been discarded while searching for relevant journals and articles.
With the help of the Boolean operator table, a framework has been developed for systematic analysis to evaluate the effectiveness of CT imaging techniques and MRI for diagnosing hepatic lesions. With the help of this tool, the preliminary framework for journal and article selection has been done. After that, inclusion and exclusion criteria have been included in this systematic analysis for pinpointing the area of study. This approach has helped pinpoint appropriate journals and articles for this systematic analysis. In terms of focusing on hepatic lesions, hepatocellular carcinoma, liver hemangioma liver cysts and nodular hyperplasia have been considered as additional keywords. Liver lesions have been considered as the alternative keyword for searching and articles on liver cirrhosis and fatty liver have been discarded. On the other hand, in terms of focusing on CT imaging techniques, direct X-ray imaging has been discarded from consideration. Similarly, T1 and T2-weighted MRI have been considered and biopsy has been discarded from consideration to pinpoint systematic review to a proper pathway. With the help of this data filtration tool, proper and effective journals and articles for this systematic analysis have been considered from relevant databases for generating an impactful concluding statement.
2.2 Inclusion and exclusion criteria
|
Factors |
Inclusion criteria |
Exclusion criteria |
|
Types of datasets |
Primary data analysis, thematic analysis, systematic review, meta-analysis, experimental research |
Informal articles and journals, blogs |
|
Year of publication |
2018-2022 |
Articles and journals before 2018 |
|
Quality evaluation |
Critical evaluation of CT and MRI for hepatic lesions diagnosis |
Abrupt and vague overview of CT and MRI for hepatic lesions diagnosis |
|
Language |
English |
Other than English |
|
Topics |
CT imaging, MRI, hepatic lesions |
fMRI, x-ray, liver cirrhosis |
|
Database |
PubMed, Google Scholar, NCBI, Research gate |
Cinahl, Proquest |
Table 3: Inclusion and exclusion criteria
With the help of the above-mentioned inclusion and exclusion criteria, datasets have been considered in this research from relevant databases mentioned above. As per inclusion criteria, some of the relevant journals and articles have been considered in this research to proceed with a systematic review of CT and MRI for diagnosing hepatic lesions.
In this systematic analysis, scholarly journals and articles have been considered that have focused on primary data analysis, thematic analysis, systematic review, experimental research, and meta-analysis. However, informal articles, journals, and blogs have been discarded from consideration. Besides, the articles in the range of 2018-2022 focusing on CT and MRI for diagnosing hepatic lesions have been considered in this systematic analysis. Scholarly journals and articles before 2018 have not been considered in this study to focus on recent viewpoints on MRI and CT for detecting and diagnosing hepatic lesions. On the other hand, such scholarly journals and articles have been considered, in which there is a critical evaluation of MRI and CT imaging techniques for hepatic lesion diagnosis.
Journals and articles with a vague overview of CT and MRI have been discarded from consideration as the systematic analysis is focused on precise analysis of the effectiveness of CT and MRI for diagnosing hepatic lesions and determining their stages. Scholarly journals and articles have been chosen from authentic databases, such as PubMed, Google Scholar, Research Gate, and NCBI. However, journals and articles have been avoided from being collected from databases, such as Cinahl and Proquest. Journals in languages other than English have been discarded from consideration as those journals and articles are not easy to access. Irrelevant topics, such as fMRI, x-ray imaging technique, or ultrasonography have been discarded from consideration as those can not be aligned with the topic of systematic analysis. With the help of this filtration tool, effective datasets have been extracted from authentic databases.
2.3 Justification of filtration tools
With the above-mentioned filtration tools, primary and secondary layers of data filtration have been done for collecting relevant datasets from scientific databases. Again, with the help of the PRISMA tool, the final layer of filtration will be done to consider a wide range of scholarly journals and articles for systematic review. With the help of the primary filtration tools, a standard framework has been set in the systematic analysis for considering effective research articles for proceeding with the analysis. This way, the systematic analysis will focus on the effectiveness evaluation of CT and MRI for diagnosing hepatic lesions.
2.4 PRISMA framework
Plenty of datasets have been considered from scientific databases, such as Google Scholar, PubMed, Research Gate, and NCBI. All the articles and journals have been clustered and inaccessible articles have been discarded from the cluster for gathering datasets. On the other hand, some articles and journals have been discarded from the cluster to prevent repetition in the systematic review. After that stage, irrelevant articles and journals were discarded from the group to gather relevant journals and articles for systematic review. With the help of the PRISMA framework (Preferred Reporting Items for Systematic Reviews and Meta-Analyses), this filtration has been done and finally, 10 scholarly journals have been considered for this research for evaluating the effectiveness of CT and MRI for diagnosing hepatic lesions.
At the very first stage, a total of 80 research articles and journals have been chosen on CT and MRI techniques for categorizing and diagnosing hepatic lesions. Among those 80 scholarly journals, 10 of them have been collected from PubMed and another 10 have been collected from Research Gate. From Google Scholar and NCBI, respectively 45 and 15 journals on the respective topic have been found. Those articles and journals have been jotted down and their accessibility has been checked. Among those journals, it can be seen that 20 journals consist only of the abstract of the research. Thus, those 20 journals have been discarded from consideration and proceeded with 60 remaining journals. Then, 20 identical journals have been discarded from consideration. After that, from that bunch of journals and articles, 10 of them have been excluded for irrelevant topics, which are not aligned with the topic of the systematic review. Thus, 10 scholarly journals have been considered in this systematic review for evaluating the effectiveness of CT imaging techniques and MRI for diagnosing hepatic lesions.
|
|||||||||||
|
|
||||||||||
3. Data extraction
3.1 MMAT tools for data extraction
The mixed method appraisal tool (MMAT) is a useful tool for appraising the quality of studies under the hood of the systematic review. With the help of this tool, the quality of the studies has been maintained in this systematic review in terms of focusing on the effectiveness evaluation of CT imaging and MRI for diagnosing hepatic lesions.
With the help of this tool, datasets have been extracted and categorized from the cluster of datasets. Those datasets have been clustered into qualitative, quantitative, and mixed methods as per the quality of the studies (Archibald et al. 2021). This tool has helped to overcome challenges, which can be seen in data extraction and filtration. Thus, the MMAT tool has been utilized in the systematic review for extracting pre-existing studies in terms of maintaining their quality. The tool has helped maintain the quality of qualitative research, quantitative descriptive studies, randomized controlled trials, and mixed methodological approaches. Thus, with the help of this tool, the integrity of the selected articles and journals can be maintained by focusing on the effective evaluation of CT imaging techniques and MRI for diagnosing hepatic lesions.
3.2 Data extraction table
|
No. |
Author |
Keywords |
Purpose |
Study design |
Sample and population |
Main findings |
|
1 |
(An et al. 2019) |
Hepatocellular carcinoma, MRI, CT, contrast media |
The prime purpose of the study is to evaluate the diagnostic accuracy of dynamic CT and MRI for diagnosing liver lesions |
Retrospective multicenter study design |
A total of 231 hepatic lesions have been evaluated in 217 patients with chronic liver disease |
Gadoxetate-enhanced MRI is superior for categorizing hepatic lesions compared to CT imaging techniques |
|
2 |
(Boyum et al. 2021) |
CT, MRI, hepatic cystic neoplasm, hepatic lesions |
The objective of the study is to identify imaging features of CT and MRI for identifying and differentiating mucinous cystic neoplasm (MCN) |
Secondary quantitative data analysis |
A total of 78 case studies, of which 22 are with MNCs and 56 are with simple biliary cysts |
CT imaging technique has helped to identify microlobulations in the cystic wall, which tended to form a clear contrasting image |
|
3 |
(Brumpt et al. 2019) |
PET, CT, MRI, hepatic lesions |
The major purpose of the study is to correlate the presence of calcifications in “alveolar echinococcosis (AE) hepatic lesions” between CT and MRI |
Primary quantitative data collection and analysis |
61 patients were considered in this study and their CT images and FDG-PET images of hepatic lesions have been analyzed |
Microcalcifications in the hepatic region can be identified with the help of CT imaging techniques more accurately. |
|
4 |
(Ganeshan et al. 2020) |
Hepatic hemangioendothelioma, CT, MRI |
The major objective of the study is to evaluate imaging features of CT and MRI for diagnosing hepatic epithelioid hemangioendothelioma (HEH) |
Primary quantitative data analysis |
The bi-institutional review identified 67 adults |
Due to the multi-layered target appearance of hepatic lesions with histopathological composition, MRI is more superior imaging technique compared to CT imaging technique |
|
5 |
(Gore et al. 2018) |
Hepatic metastases, hepatic adenoma, CT, MRI |
The major aim of the research is to evaluate the effectiveness of multidetector-row computed tomography (MDCT) for detecting liver lesions compared to MRI |
Secondary qualitative data analysis |
|
Common hepatic incidental lesions can be detected with the help of MDCT. However, for a detailed overview, MRI is more appropriate |
|
6 |
(Min et al. 2020) |
Hepatocellular carcinoma, CT, MRI |
The major objective of the study is to evaluate the effectiveness of CT and MRI for diagnosing hepatocellular carcinoma |
Primary quantitative data collection and analysis |
CT images and MRIs of 566 patients have been evaluated in this study |
Hepatic steatosis tended to decrease the performance of CT imaging, whereas, MRI is more prominent for diagnosing hepatic lesions |
|
7 |
(Rantala et al. 2020) |
CT, MRI, ultrasonography, hepatic lesions |
The prime objective of the research is to evaluate the consistency of CT and MRI for diagnosing hepatic lesions |
Primary quantitative data collection and analysis and case study analysis and evaluation |
167 CT images and 69 MRI images have been considered in this research |
MRI is more superior imaging technique for diagnosing hepatic lesions compared to the CT imaging technique |
|
8 |
(Wang et al. 2020) |
CT, MRI, ultrasonography, hepatic lesions |
The prime objective of the research is to evaluate the consistency of CT and MRI for diagnosing hepatic lesions |
Systematic review |
|
Among CT and MRI, MRI is the more effective imaging technique for identifying characteristics of liver lesions through the detection of arterial phase hyperenhancement |
|
9 |
(Wang et al. 2018) |
CT, MRI, hepatic lesions |
The study aims to compare values of CT and MRI for diagnosing hepatocellular carcinoma and analyzing prognostic factors |
Primary quantitative data analysis |
300 individuals were considered in this research |
MRI is superior compared to CT imaging technique in specificity, sensitivity, and accuracy |
|
10 |
(Xu et al. 2018) |
Hepatic hemangioma, CT, MRI |
The objective of the study is to investigate the effectiveness of CT and MRI for diagnosing hepatic hemangioma |
Primary quantitative data analysis and case study |
45 children with infantile hepatic hemangioma |
MRI is superior compared to CT imaging technique in specificity, sensitivity, and accuracy |
Table 4: Data extraction table
3.3 Summary of data extraction
From the data extraction table, it can be seen that the majority of the articles support that MRI is a more efficient imaging technique for diagnosing hepatic lesions. In oncology patients, multidetector-row computed tomography (MDCT) is the most effective imaging technique for identifying metastatic diseases. As hepatic lesions are identified through this technique, immediate management strategies can be implemented under the hood of therapeutic and prognostic implications (Gore et al. 2018). Contrast-enhanced computed tomography and MRI are the most commonly used imaging techniques for diagnosing hepatic lesions. However, after both imaging techniques, a biopsy is required to confirm carcinomas' hepatic lesions (Wang et al. 2020). On the other hand, as per the study of Boyum et al. (2021), CT generates an upper hand for identifying the presence of septations and determining the relationship of cyst wall with septations in hepatic lesions. The imaging feature of a CT scan can cause septations from microlobulations, which tend to determine hepatic lesions more accurately. However, as per Rantala et al. (2020), being severely expensive, CT scans are considered a primary confirmatory imaging technique for detecting hepatic lesions. However, in terms of providing accurate results through proper contrast differentiation, MRI is used at the later stage of diagnosis for hepatic lesions.
Similarly, both CT and MRI are effective imaging techniques and effective diagnostic indicators for infantile hepatic hemangioma (IHH). However, MRI always gains the upper hand in determining hepatic lesions more accurately due to its contrasting imaging techniques compared to CT scans (Xu et al. 2018). As per the study of An et al. (2019), it can be seen that Gadoxetate-enhanced MRI can showcase accuracy in indicating hepatic malignancies compared to dynamic CT imaging techniques. Hepatocellular carcinoma can be indicated with the help of an MRI accurately. In terms of screening small HCC (hepatocellular carcinoma), the accuracy of MRI is higher than CT scans (Wang et al. 2018). With the help of T1 and T2-weighted MRI, "hepatic epithelioid hemangioendothelioma (HEH)" can be identified more accurately in terms of identifying hepatic nodules in the peripheral subcapsular region (Ganeshan et al. 2020). Hepatic steatosis has the potential to decrease the imaging performance of CT for diagnosing HCC. Thus, MRI is used for a more accurate image for diagnosing hepatic lesions (Min et al. 2020). However, micro-calcifications can be identified with the help of CT scanning at the primary diagnosing stage (Brumpt et al. 2019).
4. Quality analysis
4.1 CASP tool for quality analysis
In terms of maintaining the overall quality of the systematic analysis, a “critical appraisal skills program” (CASP) tool has been utilized. As per the checklists in this tool, the systematic review has been evaluated to analyze its effectiveness and potential for acceptability. The systematic review tends to address a focused question, which is the effectiveness evaluation between MRI and CT for diagnosing hepatic lesions (Question 1). In this research, proper journals and articles have been considered as per the PRISMA framework to evaluate the effectiveness of CT and MRI for diagnosing hepatic lesions (Question 2). Important and relevant studies have been incorporated in the systematic review for evaluating the effectiveness of imaging techniques (Question 3).
In terms of maintaining the quality of the research, a critical analysis of selected journals has been done and the result of the study has been aligned with its question for considering reasonability (Question 4,5). As per the research, it can be considered that MRI is a superior imaging technique compared to CT for diagnosing hepatic lesions (Question 6). The results of the systematic review are precise as the considered research articles do not have any risk of bias (Question 7). As the study considers that MRI is superior to CT scanning for detecting hepatic lesions, MRI can be utilized for diagnosing hepatic lesions in the local population (Question 8). In the systematic analysis, all the important outcomes have been considered and those are worth the harm and costs (Questions 9,10).
4.2 Validation of the studies
Through the CASP tool, the studies have been validated in this research. With the help of a quality analysis tool, the quality of the systematic analysis has been maintained in terms of aligning the study with its aim. The primary aim of the systematic analysis is to evaluate the effectiveness of MRI and CT for diagnosing hepatic lesions. Thus, with the help of filtration tools, effective journals and articles have been collected, which have helped the study in terms of supporting its overview. Through the help of systematic analysis, proper evaluation of imaging techniques has been done to analyze their effectiveness. Thus, datasets have been extracted from the considered generals and articles and the quality of those studies has been analyzed to establish a strong concluding statement on the effectiveness of CT and MRI for diagnosing hepatic lesions. Thus, with the help of the CASP tool, the systematic analysis has been evaluated to check its authenticity and its capacity to focus on the topic of the systematic review. However, from the evaluation of the CASP tool, it can be seen that the systematic analysis has stood out significantly well for working strategy and effectiveness analysis of MRI and CT in terms of diagnosing hepatic lesions and differentiating those.
5. Qualitative analysis
5.1 Thematic analysis
Theme 1: Effectiveness of MRI for diagnosing hepatic lesions
Magnetic resonance imaging tends to generate high intrinsic soft-tissue contrast, which helps evaluate hepatic lesions (Albiin, 2022). With the help of T1 and T2-weighted sequences, a vivid overview of liver lesions can be identified. MRI can differentiate between tissue layers, which can eventually help to indicate the degree of hepatic lesions (Rantala et al. 2020). However, MRI is used at the critical stage of diagnosis for considering the level of hepatic lesions (Wang et al. 2020). In the case of large liver lesions and liver cysts, the effectiveness of MRI can be seen as it can detect the shape and size of the cyst. The shape of the cyst can be oval, spherical, or multilobulated. In MRI diagnosis the septate along with the thickness of the cyst wall can also be generated with deep focal imaging. In patients with MRI image scanning, the location of cysts in the liver alongside the lesions was properly diagnosed and detected. In the views of Boyum et al. 2021, for MRI imaging and techniques only, the addition of mucin under the category of “heterogeneous cyst content” can be added. This is another effective feature of the MRI which helps in the accurate diagnosis.
Clinically, in most cases of solid liver lesions, MRI with the multiphase enhancement of over is done with the help of a contrasting agent called “Gadolinium-based contrast agent (GBCA)”. In this entire process, the focus is kept on the “T1 and T2 weighted images” of the liver which help in the specification of lesions (Rantala et al. 2020). One of the drawbacks of this technique is that the contrasting agent GBCA is mostly tolerated in patients but is associated with the risk of developing “nephrogenic systemic fibrosis” or some adverse body reactions. Rantala et al. 2020 have stated that in this method, it is found that liver lesions that have a “hepatocyte with intact biliary excretion mechanism” take up the contrasting agent and show vivid results of lesions.
Theme 2: Effectiveness of CT imaging technique for diagnosing hepatic lesions
CT imaging technique uses multidetector x-ray beams for diagnosing hepatic lesions (Boyum et al. 2021). However, significant contrasted images can not be formed with the help of CT imaging techniques compared to MRI. Arterial phase imaging techniques can help identify multiple tumor masses within the liver. With the help of contrast differentiation, CT imaging can detect hepatic lesions (Baron 2022). CT imaging is generally preferred when the MRI imaging is not supportive or is not effective in identifying lesion areas. A multiphase contrast-enhanced CT is done in that case to identify the hepatic lesions. Ganeshan et al. 2020 state that the multiphase involves the arterial and portal venous phases' findings which help in the detection of lesion patterns and numbers. This can be explained by two cases where a report of enhanced solitary mass in the cirrhotic liver with thrombosis of the portal vein, ascites, and splenomegaly suggested a hepatocellular carcinoma but a small peripheral and enhanced lesion in an asymptomatic female with normal liver suggested hepatic hemangioma.
One of the major advantages of CT is that it is easily accessible. The scanning through CT is easily done and the reports can be generated very quickly. So for a quick diagnosis, most physicians prefer to do a CT of the hepatic lesions (Ganeshan et al. 2020). Also, the patients do not require a long breath hold. Another advantage of CT is that the detection of the presence of gas inside a lesion can only be detected with CT, which means in cases of necrotic lesions, abscesses, or tumors the CT scan is advantageous to perform. CT can detect any cases of acute bleeding in hepatocellular carcinoma or ruptures (Brumpt et al. 2019). In Figure 4, it can be seen that the central calcification alongside a hypoattenuating liver is detected in the portal venous image of a CT scan, but only hypo enhancing is detected in the other image and no calcification is seen. This image is the detection done through MRI (Brumpt et al. 2019). Therefore, it can be said that in cases of hepatocellular carcinoma or HCC, the diagnosis and monitoring are done through CT. CT can also detect any calcification inside the liver, that is the presence of calcified metastases, calculi, hematoma, or hydatid disease.
Theme 3: MRI is a superior imaging technique for diagnosing hepatic lesions compared to the CT imaging technique
Among MRI and CT imaging techniques, MRI is more effective to evaluate the degree of hepatic lesions (Wang et al. 2018). With the help of soft tissue contrasting factors, MRI can detect the degree of hepatic lesions. It can also be said that MRI is preferred over CT because no kind of radiation is involved. Also, an unenhanced MRI is performed in the case of pregnant women which is safer than CT. An MRI scan provides better tissue characterization than a CT. In the case of Focal nodular hyperplasia, MRI detection is considered to be superior to CT because of hepatobiliary contrast agents. According to Wang et al. 2018, in the case of MRI, only the detection of microscopic fat in the case of hepatocellular carcinoma or hepatocellular adenoma is possible.
A major feature of hepatocellular carcinoma is the appearance of a capsule which might be delayed in many cases. MRI is the only possible way through which this capsular appearance can be detected (Gore et al. 2018). The use of contrasting agents in MRI improves the detection of small metastases that are less than 1 cm. However, the wind of extremely small metastatic lesions goes unnoticed in the case of CT scans. In the views of Gore et al. 2018, in peripheral cholangiocarcinoma, the longitudinal extensions can be more accurately detected with the help of MRI than CT. So, it shows that the MRI technique is more advantageous than CT due to its wide applicability, hyper-contrasting capabilities, and accurate detection. The major drawback of CT is the radiation that is being used (An et al. 2019). In the case of hepatic carcinoma, this radiation is not beneficial and poses further risks of cell damage. Also, the majority of physicians avoid the risk of using CT in case of hepatic lesions because of the risk of contrast nephropathy (An et al. 2019). However, there are certain cons of using MRI in special cases like ascites. In the case of ascites, the image that is generated through MRI is lower in quality and not proper for diagnosis. Hence, in that case, CT is preferred over MRI.
5.2 Findings
Among MRI and CT scanning, MRI is superior for diagnosing hepatic lesions. In the case of MRI, it was found that MRI has multiple benefits over CT. The effectiveness of CT is found to be in special cases in comparison to MRI. In the case of large liver lesions, MRI images are found to be clearer and can be differentiated into tissue layers. MRI has an advantage over CT because of the contrasting agents (Min et al. 2020). Several contrasting agents are developed for different MRI techniques which are easily taken up by the hepatocytes. The first agent was called Teslascan and later two vastly used agents came into the market called “Gadolinium (Gd)-BOPTA (MultiHance) and Gd-EOB-DTPA (Eovist Injection)” (Min et al. 2020). The use of these contrasting agents helps to produce differentiated images which help to detect the layers as the layer that is affected easily takes up color due to more intensity and cell division process. MRI is also preferred because of its techniques and it is safer to use on pregnant women.
In the case of a hepatic abscess, the imaging feature of MRI depends on the progression of lesions. In situations with early lesions, a CT scan seems to be beneficial as it appears like a heterogeneous tissue mass while in a mature one, it appears as a hypoattenuating necrotic gas-filled center with an enhanced rim. Brumpt et al. 2019 have supported the fact that HCA appears difficult to diagnose especially with CT as they have a similar appearance to benign and malignant tumors. However, MRI is found to be effective in diagnosing HCA and its subtypes (Brumpt et al. 2019). In the case of inflammatory HCAs, a very high SI is demonstrated on T2WI and is shown to be hyper-enhanced in the arterial phase. This particular feature has 85 to 88% sensitivity and is almost 90 to 100% accurate for inflammatory HCAs (Wang et al. 2020). However, β- catenin HCA and other HCA that are unclassified do not have any imaging features for MRI. Contrarily in the case of metastasis, CT is the preferred image modality for the initial diagnosis process, assessment, and surveillance. It is because CT provides a greater overview of the primary tumor and also shows the other potential sites for metastases (Wang et al. 2020).
Magnetic resonance is found to be useful in the planning process of resection of metastasis and cases of severe pancreatic cancer. In the reports presented by Xu et al. 2018, it was found that a hepatobiliary contrast agent called gadoxetic acid produced enhanced MRI images that had a sensitivity of 86% in case of colorectal hepatic metastases in comparison to contrasted CT scans. It is said that gadoxetic acid in combination with enhanced MRI has the highest sensitivity for the detection of hepatic metastases. A known limitation, liver steatosis, is used for the assessment of “small hypoattenuating metastases on CT” and so in this case MRI acts as a problem-solving tool (Xu et al. 2018). In the findings, it can be said that both CT and MRI have been widely explored for the detection of lesions, metastases, necrosis, and other hepatocellular dysfunctions. The availability of CT is more than MRI and the scanning period is comparatively shorter (Gore et al. 2018). However, the contrasting field and resolution is better and enhanced in the case of MRI and thus are preferred over CT in most of the cases. So, it can be said that the effectiveness of MRI is more than CT in the case of hepatic lesions and other carcinomas.
6. Quantitative synthesis
Figure 14: Heterogeneity in studies with primary quantitative datasets
|
Study |
Event |
Sample Size |
Outcome |
SE |
CI Lower (Var) |
CI Upper (Individual Weights) |
|
(An et al. 2019) |
1 |
217 |
0.004608294931 |
0.004608294931 |
0.00002123638217 |
47089 |
|
(Boyum et al. 2021) |
2 |
78 |
0.02564102564 |
0.01813094311 |
0.000328731098 |
3042 |
|
(Brumpt et al. 2019) |
1 |
61 |
0.01639344262 |
0.01639344262 |
0.000268744961 |
3721 |
|
(Ganeshan et al. 2020) |
2 |
67 |
0.02985074627 |
0.02110766511 |
0.0004455335264 |
2244.5 |
|
(Min et al. 2020) |
1 |
566 |
0.001766784452 |
0.001766784452 |
0.000003121527301 |
320356 |
|
(Rantala et al. 2020) |
2 |
236 |
0.008474576271 |
0.005992430349 |
0.00003590922149 |
27848 |
|
(Wang et al. 2018) |
1 |
300 |
0.003333333333 |
0.003333333333 |
0.00001111111111 |
90000 |
|
(Xu et al. 2018) |
1 |
45 |
0.02222222222 |
0.02222222222 |
0.0004938271605 |
2025 |
Table 5: Analysis of datasets with primary quantitative data
As per the analytical approach, it can be identified that dispersion in the datasets is significantly low, and the high-class interval upper (CI upper) value indicates the weight of the studies, which eventually indicates the acceptability of the datasets and it also indicates low risk of bias in the studies.
From the quantitative analysis, it can be seen that the standard error and variance of all journal articles, consisting of primary quantitative data analysis, showcase a restricted area of diversification. This approach can be helpful in terms of identifying the risk of bios in the research articles. The validity of the research articles is represented by the weightage of the articles, which is indicated by the CI upper value. Standard error and variance tend to determine heterogeneity in the studies. This factor significantly helps in distinguishing acceptance levels of generals and articles for the systematic review. In this quantitative analysis, a variety of events, which have been incorporated in the studies, mentioned in the tabular form have been identified with the sample size. The outcome of the research is calculated by dividing the prior-mentioned aspects. From the analytical approach, it can be seen that standard errors in the selected studies are significantly lower, as the values have been compared in a standard range. However, the range of data variance has shifted slightly due to differences in clusters of datasets, compared to the actual population. Both standard error and outcome are expanded than the cluster of the data pool. However, the risk of bias in journals with quantitative analysis is significantly low, as there is no trace of data manipulation or adversities in data handling. Thus, the acceptance range of the journals is significantly high.
The majority of the studies in the systematic analysis have conducted research and collected data sets from a single event. Thus, the probability of errors in the data sets is significantly low. However, three of the selected journals have indicated acceptance of datasets from more than one event. Those studies have considered proper ethical approaches to handle datasets without any risk of bias. Thus, the level of acceptance is significantly higher for those datasets in the systematic analysis. Those datasets have helped the research to analyze the effectiveness of CT and MRI for diagnosing hepatic lesions through quantitative approaches. As the datasets showcase high weightage in terms of their acceptability factor, the standard error of those datasets is significantly low (Nicholson et al. 2019). On the other hand, quantitative analysis of the datasets has exposed that all the journals and articles consisting of primary quantitative data sets are acceptable for this systematic analysis for the effectiveness evaluation of CT imaging techniques and MRI for diagnosing hepatic lesions.
7. Discussion and conclusion
7.1 Inferences for addressing research questions
Qualitative analysis
Quantitative datasets in the research do not signify any risk of bias in the studies, which effectively indicates that MRI is a more prominent imaging technique for diagnosing hepatic lesions compared to CT imaging techniques. From the thematic analysis, the information gathered shows that MRI is more effective in gathering data about hepatic lesions and carcinomas. It was seen that the qualitative analysis presented many sides of both MRI and CT in the field of hepatic lesions and carcinomas. The three thematic analyses presented that MRI can detect the differentiation of hepatic lesions and sites. Along with this, the effectiveness of MRI is seen in its ability to detect the shape and size of the cyst. The addition of mucin for heterogeneous cysts can only be added in the case of MRI diagnosis processing but not in CT (Gore et al. 2018). Hyper Contrasting capabilities of MRI make it more accurate than CT. Also, MRI can be done with lesser frequency in case of the pregnant women and is found to impact less on the developing fetus. CT uses radiation and can pose a serious threat to the developing womb leading to genetic alterations and developing defects (An et al. 2019).
The advantages of CT can be counted in the case of necrotic lesions and tumors where the detection of the presence of gas inside a lesion can only be detected with CT. This means in cases of necrotic lesions, abscesses, or tumors the CT scan is advantageous to perform. Also, CT can detect any cases of acute bleeding in hepatocellular carcinoma or ruptures (Ganeshan et al. 2020). The capsular appearance of a hepatic carcinoma is only detected with the help of MRI where the capsule is differentiated into several layers that indicate the layers which have carcinogenic cells. The carcinogenic cells appear to be darker under the influence of the contrasting agent and produce a deeper and darker field. This process is not obtained in the case of CT (Ganeshan et al. 2020). Hence the major advantage of using MRI is the use of contrasting agents which makes it more acceptable and accurate. The sensitivity of the MRI tools for the diagnosis of HCAs, lesions, and carcinomas is way more than that of CT (Wang et al. 2020).
From the systematic review, it can be considered that MRI is superior compared to CT imaging techniques in terms of its effectiveness in diagnosing hepatic lesions. Lesions can be detected along with their shape, size, effective area, and potential sites where the tissues might be affected (Albin, 2022). The MRI seems to be a noble process with more effective results in hepatic lesions than CT and hence is preferred and used as a diagnostic tool.
Quantitative analysis
From the quantitative analytical approach, it can be seen that the majority of the studies consisting of primary quantitative data sets are acceptable in the systematic analysis as their weightage is significantly higher. Thus, the standard error of the data sets is lower and the datasets are in the level of acceptance. On the other hand, the risk of bias in those datasets is significantly low and this factor makes the studies appropriate for the research. The heterogeneity of the research articles is comparatively low and the articles consisting of primary quantitative data sets tend to justify research questions and establish a significant concluding statement regarding the effective evaluation of CT and MRI for diagnosing hepatic lesions. Besides, from the analytical approach it can be seen that, due to proper ethical consideration maintenance, the risk of bias in those datasets is considerably low, which makes the journals and articles acceptable for systematic analysis.
7.2 Conclusion
From the analytical approach in the systematic analysis, it can be considered that MRI is a more effective imaging technique for detecting the microscopic levels of hepatic lesions. With the hyper-contrasting capabilities of MRI, images of hepatic relations can be seen perfectly. The shape and size of hepatic cysts can be detected with the help of an MRI. From the analytical approach, it can be seen that the contrasting capability of magnetic resonance imaging is more accurate than computed tomography. However, the CT imaging technique can detect acute bleeding in case of hepatocellular carcinoma. In this case, CT can differentiate different layers of hepatic tissues for determining hepatic lesions. However, minute hepatic lesions can be properly detected with the help of MRI instead of CT scans. Thus, MRI is used as a confirmatory imaging technique after CT scanning for diagnosing hepatic lesions. Besides, pricing is a significant factor to be considered for diagnosing hepatic lesions. MRI is significantly costly, compared to CT scans and provides better accuracy. Through MRI, the capsular appearance of hepatic lesions can be detected effectively, which makes it a superior imaging technique to CT. In peripheral cholangiocarcinoma, the longitudinal extensions can be more accurately detected with the help of MRI than CT. So, it shows that the MRI technique is more advantageous than CT due to its wide applicability, hyper-contrasting capabilities, and accurate detection. It can be said that both CT and MRI have been widely explored for the detection of lesions, metastases, necrosis, and other hepatocellular dysfunctions. However, both imaging techniques have their advantages and disadvantages in relevant fields. However, in terms of diagnosing hepatic lesions, MRI is a superior technique. Though CT can detect images of micro lesions, this is incapable of detecting large lesions in hepatic lobules. Thus, MRI is prioritized as it uses a contract-enhancing strategy for detecting large hepatic lesions.
7.3 Limitations
In terms of proceeding with the systematic analysis, some limitations have been faced, which are significant in the research. Limited datasets are available in scientific databases pinpointing the effectiveness of MRI and CT imaging for detecting hepatic lesions. The cases of hepatic lesions alone are lacking and hence in many cases, some data have been collected from the effectivity of MRI in diagnosing carcinomas, necrotic areas, and HCAs. The study is unable to explore the different techniques of MRI which are used for different diagnoses of hepatic lesions and abnormalities. Due to the restricted availability of resources in authentic databases and the case of inclusion and exclusion criteria, a detailed comparative approach cannot be presented in the study.
7.4 Suggestions for future studies
As MRI is more effective compared to CT imaging techniques, a detailed overview analysis of multidetector CT can be done in the future to evaluate its effectiveness for diagnosing hepatic lesions. Besides, ultrasonography can also be considered in studies for detecting hepatic lesions and this can be compared with CT and MRI. In terms of evaluating the effectiveness of CT and MRI for diagnosing hepatic lesions, experimental studies can be more effective. However, a comparison can be done between ultrasonography and CT to evaluate their effectiveness in diagnosing stages of hepatic lesions.
References
ALBIIN, N., 2022. MRI of Focal Liver Lesions. Current Medical Imaging, vol. 8, no. 2, pp. 107–116.
ALLAN, M., ASIMAKIDOU, M. AND DAVENPORT, M. (2020). Antenatally-detected liver cysts: Causes and characteristics, indications for intervention. Journal of Pediatric Surgery, 55(3), pp.441–445. doi:10.1016/j.jpedsurg.2019.03.023.
ARCHIBALD, M., WIEBE, S., RIEGER, K., LINTON, J., and WOODGATE, R., 2021. Protocol for a systematic review of living labs in healthcare. BMJ Open, vol. 11, no. 2, p. e039246, [Available from DOI 10.1136/bmjopen-2020-039246].
AZIZADDINI, S. and MANI, N. (2021). Liver Imaging. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK557460/.
BARON, R., 2022. The Radiology Assistant: Characterisation of liver masses. [online]. radiologyassistant.nl Available from: https://radiologyassistant.nl/abdomen/liver/characterisation-of-liver-masses.
CLEVELAND CLINIC, 2022. Liver Lesions: Types, Causes, Symptoms & Treatment. [online]. Cleveland Clinic Available from: https://my.clevelandclinic.org/health/diseases/14628-liver-lesions#:~:text=Liver%20lesions%20are%20abnormal%20growths [viewed 26 October 2022].
EGHLIMI, H., ARASTEH, P., and AZADE, N., 2020. Orthotopic liver transplantation for Management of a Giant Liver Hemangioma: a case report and review of the literature. BMC Surgery, vol. 20, no. 1, [Available from: DOI 10.1186/s12893-020-00801-z].
ENDO, T., KOIKE, Y., KANAYAMA, M., SUZUKI, R., FUJITA, R., YAMADA, K., IWATA, A., HASEBE, H., SUDO, H., IWASAKI, N. AND TAKAHATA, M. (2022). Distinct progression pattern of ossification of the posterior longitudinal ligament of the thoracic spine versus the cervical spine: a longitudinal whole-spine CT study. Journal of Neurosurgery: Spine, pp.1–8. doi:10.3171/2022.1.spine211010.
ENDO, Y., SHIMAZU, M., SAKURAGAWA, T., UCHI, Y., EDANAMI, M., SUNAMURA, K., OZAWA, S., CHIBA, N., and KAWACHI, S., 2022. Successful treatment with laparoscopic surgery and sequential multikinase inhibitor therapy for hepatocellular carcinoma: A case report. World Journal of Gastrointestinal Surgery, vol. 14, no. 3, pp. 260–267, [Available from DOI 10.4240/wjgs.v14.i3.260].
GANGAHDAR, K., SANTHOSH, D., and CHINTAPALLI, K.N., 2018. MRI Evaluation of masses in the noncirrhotic liver. [online]. www.appliedradiology.com Available from: https://www.appliedradiology.com/articles/mri-evaluation-of-masses-in-the-noncirrhotic-liver.
GORE, R.M., THAKRAR, K.H., WENZKE, D.R., NEWMARK, G.M., MEHTA, U.K., and BERLIN, J.W., 2017. That liver lesion on MDCT in the oncology patient: is it important? Cancer Imaging, vol. 12, no. 2, pp. 373–384, [Available from: DOI 10.1102/1470-7330.2012.9028].
KOW, A.W.C. (2019). Hepatic metastasis from colorectal cancer. Journal of Gastrointestinal Oncology, 10(6), pp.1274–1298. doi:10.21037/jgo.2019.08.06.
KOW, A.W.C., 2019. Hepatic metastasis from colorectal cancer. Journal of Gastrointestinal Oncology, vol. 10, no. 6, pp. 1274–1298, [Available from DOI 10.21037/jgo.2019.08.06].
MCGLYNN, K.A., PETRICK, J.L., and EL‐SERAG, H.B., 2020. Epidemiology of Hepatocellular Carcinoma. Hepatology, [Available from DOI 10.1002/hep.31288].
NATIONAL INSTITUTE OF BIOMEDICAL IMAGING AND BIOENGINEERING, 2018. Magnetic Resonance Imaging (MRI). [online]. National Institute of Biomedical Imaging and Bioengineering Available from: https://www.nibib.nih.gov/science-education/science-topics/magnetic-resonance-imaging-mri.
NICHOLSON, B.D., AVEYARD, P., HAMILTON, W., BANKHEAD, C.R., KOSHIARIS, C., STEVENS, S., HOBBS, F.R., and PERERA, R., 2019. The internal validation of weight and weight change coding using weight measurement data within the UK primary care Electronic Health Record. Clinical Epidemiology, vol. Volume 11, pp. 145–155, [Available from DOI 10.2147/clep.s189989].
RATINI, M., 2022. What Are Liver Lesions? [online]. WebMD Available from: https://www.webmd.com/hepatitis/liver-lesions [viewed 16 April 2021].
RAWLA, P., SUNKARA, T., MURALIDHARAN, P., and RAJ, J.P., 2019. An updated review of cystic hepatic lesions. Clinical and Experimental Hepatology, vol. 5, no. 1, pp. 22–29, [Available from: DOI 10.5114/ceh.2019.83153].
SHREENATH, A.P. and KAHLOON, A., 2022. Hepatic Adenoma. [online]. PubMed Available from: https://www.ncbi.nlm.nih.gov/books/NBK513264/#:~:text=Hepatic%20adenomas%20are%20benign%20liver [viewed 29 October 2022].
US FOOD AND DRUG ADMINISTRATION, 2020. What is Computed Tomography? FDA.
VENTURI, A., PISCAGLIA, F., VIDILI, G., FLORI, S., RIGHINI, R., GOLFIERI, R., and BOLONDI, L., 2017. Diagnosis and management of hepatic focal nodular hyperplasia. Journal of Ultrasound, vol. 10, no. 3, pp. 116–127, [Available from DOI 10.1016/j.jus.2007.06.001].
WANG, G., ZHU, S., and LI, X., 2018. Comparison of values of CT and MRI imaging in the diagnosis of hepatocellular carcinoma and analysis of prognostic factors. Oncology Letters, vol. 17, no. 1, [Available from DOI 10.3892/ol.2018.9690].
Journals
AN, C., LEE, C.H., BYUN, J.H., LEE, M.H., JEONG, W.K., CHOI, S.H., KIM, D.Y., LIM, Y.-S., KIM, Y.S., KIM, J.H., CHOI, M.S., and KIM, M.-J., 2019. Intraindividual Comparison between Gadoxetate-Enhanced Magnetic Resonance Imaging and Dynamic Computed Tomography for Characterizing Focal Hepatic Lesions: A Multicenter, Multireader Study. Korean Journal of Radiology, vol. 20, no. 12, p. 1616, [Available from DOI 10.3348/kjr.2019.0363].
BOYUM, J.H., SHEEDY, S.P., GRAHAM, R.P., OLSON, J.T., BABCOCK, A.T., BOLAN, C.W., MENIAS, C.O., and VENKATESH, S.K., 2021. Hepatic Mucinous Cystic Neoplasm Versus Simple Biliary Cyst: Assessment of Distinguishing Imaging Features Using CT and MRI. American Journal of Roentgenology, vol. 216, no. 2, pp. 403–411, [Available from DOI 10.2214/ajr.20.22768].
BRUMPT, E., BLAGOSKLONOV, O., CALAME, P., BRESSON-HADNI, S., VUITTON, D.A., and DELABROUSSE, E., 2019. AE hepatic lesions: correlation between calcifications at CT and FDG-PET/CT metabolic activity. Infection, vol. 47, no. 6, pp. 955–960, [Available from DOI 10.1007/s15010-019-01328-z].
GANESHAN, D., PICKHARDT, P.J., MORANI, A.C., JAVADI, S., LUBNER, M.G., ELMOHR, M.M., DURAN, C., and ELSAYES, K.M., 2020. Hepatic hemangioendothelioma: CT, MR, and FDG-PET-CT in 67 patients—a bi-institutional comprehensive cancer center review. European Radiology, vol. 30, no. 5, pp. 2435–2442, [Available from DOI 10.1007/s00330-019-06637-3].
GORE, R.M., THAKRAR, K.H., WENZKE, D.R., NEWMARK, G.M., MEHTA, U.K., and BERLIN, J.W., 2018. That liver lesion on MDCT in the oncology patient: is it important? Cancer Imaging, vol. 12, no. 2, pp. 373–384, [Available from: DOI 10.1102/1470-7330.2012.9028].
MIN, J.H., KANG, T.W., KIM, Y.-Y., CHA, D.I., KIM, Y.K., KIM, S.H., SINN, D.H., HA, S.Y., and KIM, K., 2020. Vanishing washout of hepatocellular carcinoma according to the presence of hepatic steatosis: diagnostic performance of CT and MRI. European Radiology, vol. 31, no. 5, pp. 3315–3325, [Available from DOI 10.1007/s00330-020-07438-9].
RANTALA, E.S., PELTOLA, E., HELMINEN, H., HERNBERG, M., and KIVELÄ, T.T., 2020. Hepatic Ultrasonography Compared With Computed Tomography and Magnetic Resonance Imaging at Diagnosis of Metastatic Uveal Melanoma. American Journal of Ophthalmology, vol. 216, pp. 156–164, [Available from DOI 10.1016/j.ajo.2020.03.049].
WANG, D.C., JANG, H.-J., and KIM, T.K., 2020. Characterization of Indeterminate Liver Lesions on CT and MRI With Contrast-Enhanced Ultrasound: What Is the Evidence? American Journal of Roentgenology, vol. 214, no. 6, pp. 1295–1304, [Available from DOI 10.2214/ajr.19.21498].
WANG, G., ZHU, S., and LI, X., 2018. Comparison of values of CT and MRI imaging in the diagnosis of hepatocellular carcinoma and analysis of prognostic factors. Oncology Letters, vol. 17, no. 1, [Available from DOI 10.3892/ol.2018.9690].
XU, M., PAN, F., WANG, W., ZHANG, X., Li, X., HONG, Y., ZHOU, L., XIE, X., and LYU, M., 2018. The value of clinical and ultrasound features for the diagnosis of infantile hepatic hemangioma: Comparison with contrast-enhanced CT/MRI. Clinical Imaging, vol. 51, pp. 311–317, [Available from DOI 10.1016/j.clinimag.2018.06.017].