- Effective Reporting And Record Keeping In Health And Social Care Services
- LO1: Legal and regulatory aspects of reporting and record-keeping in a care setting
- LO2: Internal and external recording requirements in a care setting
- LO3: Use of technology in reporting and recording service user care
- LO4: Keeping and maintaining records in a care setting in line with national and local policies and appropriate legislation
Effective Reporting And Record Keeping In Health And Social Care Services
The UK’s top-notch online assignment help, Native Assignment Help, specialises in providing unparalleled quality and outstanding customer satisfaction through our human-written case study. Our dedicated team can readily assist you with challenging essays or intricate research papers. Choose Native Assignment Help today and experience first-hand what a reliable and committed partner can achieve for you.
LO1: Legal and regulatory aspects of reporting and record-keeping in a care setting
Consequences of non-compliance
Non-compliance in a healthcare setting implies violation of laws and rules related to healthcare practice in a particular setting. In this case, Mrs Jones has been visiting the A&E department for the third time in three months for injuries which she claims were accidental. If she is an assault victim, crossing regulatory barriers and approaching her to reveal her truth would endanger her and her son’s life. Hence, the safety of service users is being compromised, which is not ideal. The media could be used as an effective tool to expose assaulters and can also be used to capture the attention of several NGOs that work to support assault victims (Morris et al., 2021). However, approaching the media would be non-compliance in this case and might hamper the credibility of the hospital.
Regulatory implications of non-compliance
Most major legal implications of non-compliance involve penalties, which include hefty fines. These fines can cause the erosion of the huge profits of reviewed organisations and make the smaller ones get completely wiped off the industry (IPSOS MORI, 2013). Apart from that, reputational damage is unavoidable and that might demand additional audits, If the audits reveal the reason behind the non-compliance is not very significant, the repercussions in such cases would be huge. Finally, non-compliance might even lead to imprisonment or other legal actions that would hamper the career of a professional or the healthcare setting might be shut down completely.
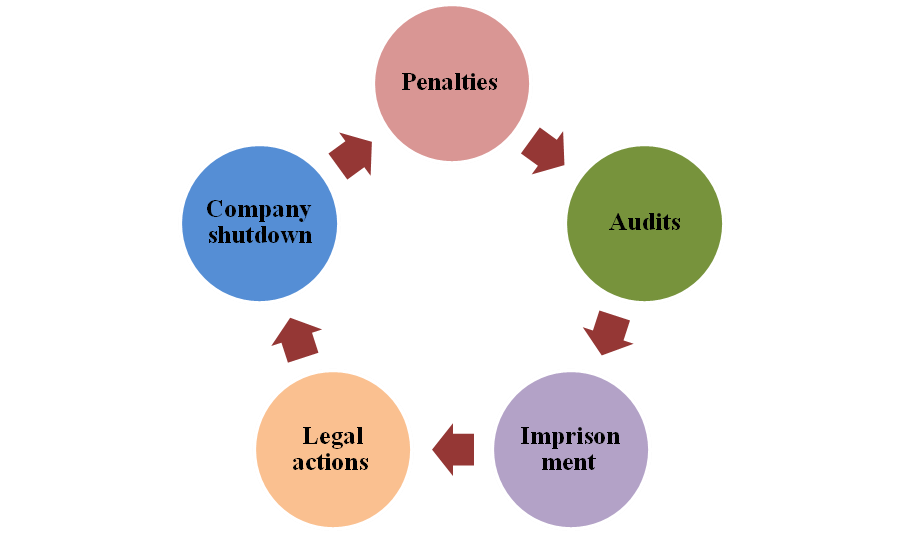
Figure 1: Implications of non-compliance
Regulatory requirements in record-keeping
Regulatory requirements regarding record-keeping in a hospital setting in the UK have been mentioned under Regulation 17 of “Care Quality Commission(CQC)”.
- It has been mentioned that providers are required to maintain accurate, detailed and complete patient records.
- Also, records related to staff employment and overall management are to be maintained (Cqc, 2023). Under a complete record of any service user, their care and treatment would have to be outlined along with related decisions. This would include consent records along with reasons behind changes being made in them.
- It has been outlined that both paper and electronic forms of record could be kept, including that they meet the requirements of the “Data Protection Act 2018” (Scott, 2004).
- Also, evidence of decision-making on behalf of service users who lack the ability to make their own decisions would have to be recorded.
- Records on management of regulated activities like planning and delivery of healthcare.
- Governance arrangements records, policies, service maintenance records and audits or reviews are included in the list.
- Feedback provided by service users would also need to be recorded.
- Most importantly, every record would have to be securely stored, as listed under 17C.
Statutory requirements
- “Data Protection Act 2018”: Rules regarding the prevention of breach of personal confidential information of service users have been listed under this act under several policies and procedures.
- “Human Rights 1998”: “European Convention on Human Rights” has been emphasised under this law (Ico, 2018, a). Specifically, Articles 8 and 5 of the Act have been emphasised and the set of rights regarding private information of citizens has been mentioned.
- “Information Commissioner's Office Data Sharing Code of Practice (ICO, 2016)”: Sections 52D and 52A of the act have listed several legal requirements regarding record-keeping.
LO2: Internal and external recording requirements in a care setting
Evaluation of own work setting
Patient data in the healthcare setting involves both paper documents and electronic records, depending on the situation. As mentioned by Scott et al. (2021), paper documents eliminate the risk of a data breach, but storing these data is a potential problem. The fact that Mrs Jones had visited the healthcare setting a third time has been obtained from existing data. The records have shown that she had been admitted earlier with different injuries but each time she mentioned them as accidental. However, this information had been obtained from electronic records of previous months and not paper ones. One point that has been missing from records of Mrs Jones is her treatment options. As opined by Zulkipli et al. (2022), an adequate diagnosis brings out the reasons behind an injury or health problem. The choice made by Mrs Jones regarding her diagnosis options would reveal whether she wants the actual reason to be revealed but that has not been the case. Hence, it might be recommended that preferable treatment options chosen by the service user are mentioned in future records.
Examining the care-setting processes
Patient records can be shared under certain circumstances, provided that the patients themselves approve it. As stated by Hernandez-Boussard et al. (2020), the Data Confidentiality Act provides every individual with the right to demand their personal information be kept confidential. Scenarios in which service user information in health care can be shared include research purposes or medicolegal cases when the court provides documented permission. In this health setting, it has been ensured that no service user feels violated since it is ensured that their information would not be used for other purposes without their consent. It has been suspected that Mrs Jones is a victim of the assault but under no circumstances would the hospital adhere to non-compliance in any form. As mentioned by Cave et al. (2019), in cases where the health facility suspects potential abuse of one of the patients, they might officially apply for permission from the court to inspect the patient. In this health setting, it would be ensured that Mrs Jones approves of this and based on that, the hospital would proceed towards seeking a legal investigation. Records of Mrs Jones's past two admissions would be used to get approval from the court.
Requirements in recording
Internal requirements imply the needs of the patients or service users and the care settings that are served by record keeping. These requirements are those that can be provided by the patient and the hospital. On the other hand, external requirements involve meeting regulatory requirements. These are those that are provided by the hospital to the patient and maintained in the record.
Internal requirements:
- Personal information of service users.
- Social screening.
- Genetic information.
- List of medications and vaccinations.
- Medical history of service users.
- Family health history.
- Hospital discharge summaries.
- Health insurance forms.
- Consent forms.
- Laboratory data that would include diagnostic test results.
- Diagnostic evaluation records.
- Pharmacy records.
- Billing information.
- Legal documents.
External requirements:
- Reliable computers
- Fax machines
- Printer and scanner
- Cell phones
- Paper and pen
- Hospital stamps (for paper records)
- EHR and EMRs
Reasons for sharing information
Every healthcare setting is obliged to comply with healthcare regulations, one among which is proper record-keeping. As opined by Saripalle et al. (2019), one primary necessity of maintaining the record of a patient is that it would provide a detailed overview of their health status. Based on this, their intervention could be designed, as it would be irrational to expect a professional to physically remember every piece of information about the numerous patients they are assigned. Apart from that, record-keeping would help professionals obtain a list of available services in the healthcare setting from which they would be able to choose. Overall, adequate and effective record-keeping would help ensure that service users are being provided with the right support and care and also shed a burden off the shoulders of professionals.
Within a health setting, one patient might be allocated to several professionals over their complete time. In such cases, the other doctors must have detailed information on patient summaries (Ico, 2018, b). Failing to do so might endanger the patient’s life because of a lack of information. In the case of sharing information with external bodies, the main reason might be an investigation. In this case, it has been suspected that Mrs Jones is an assault victim but the hospital alone might not be able to take any steps to prevent it. They might need to inform legal authorities and ask for their help in bringing justice. Most importantly, record-keeping saves a healthcare setting from liabilities and obligations.
Record storage process
- It is checked that the hospital is allowing only authorised staff to access medical records.
- Aligning with medical considerations: instances like deciding on how long one patient's data is to be stored or providing patient reviews while allocating them to another doctor (Nmc, 2023).
- Reviewing significant health events and medical history, including ongoing and past medications, previous surgical procedures and immunisation records.
- Ensuring that the records are available in specific situations:
- In the case of patients or their representatives themselves, request to access them.
- In the event of succeeding physical demands to access them after one physician discontinued their practice (Apa, 2023),.
- In case demanded by law.
- Transferring records to a party that had demanded.
- Charging a fair fee.
- Storing medical records after transferring.
- Informing patients about ways they could access it and the amount of time they would be provided (Keshta and Odeh, 2021).
- Verification of discarded records to predict patient confidentiality.
LO3: Use of technology in reporting and recording service user care
Effectiveness of technology use
The primary reason behind including technology in healthcare is to safeguard patient safety. As said by Almathami et al. (2020), technology has provided accurate and faster access to patient information, and EHR stands as evidence of this fact. Besides providing easy access to healthcare providers, EHRs have also saved patients from calling doctors to obtain their test results. Compared to paper documents, ensuring confidentiality is easier with EHRs. Also, technology has improved care access, which has been a significant barrier to date. Cost, limitations and distance have been some factors that have prevented patients from getting emergency care and led to delayed treatment. Telehealth is an example of how these factors are prevented from hampering the health access of patients nowadays. Some other examples include portable diagnostic tools that eliminate the requirement of travelling long distances. Finally, as mentioned by Vaishnavi et al. (2019), technological advancements have made diagnostics more accurate, faster and more accessible. Chronic illnesses can now be screened faster, preventing further health risks.
Review of using digital technology
Digital technology lowers healthcare costs and prevents further diseases. Besides, they help the patients monitor their chronic conditions themselves and allow the tailoring of medicines. Healthcare providers provide an extensive view of patient health through digital tools because of increased access to information. As said by Landes et al. (2020), patients are provided with greater control over their health data through digital technology, and hence, medical outcomes are improved. As a revolution in healthcare, digital technology has provided a vast potential for the improvement of diagnosis and disease treatment.
Benefits of involving service users in their record-keeping
One primary advantage of involving service users in record-keeping is that communication is enhanced with the service provider. Besides, patients could provide a detailed overview of their medical history, which would not be accessible completely from the records. Most importantly, this would come in handy in court trial cases because it would help the hospital justify its roles (Scott, 2004). In this case, it would be helpful for the hospital to mention to the court that Mrs Jones had been provided with the right treatment and had made no contribution to her injuries.
Using technology in record-keeping
Primary EHR and EMRs are technological tools that are used in record keeping in health care. These are mostly used in storing patient information, including every treatment process they undergo in the healthcare setting. As mentioned by Vazirani et al. (2019), this data is later accessed by health professionals to design intervention plans. Additionally, they are used to reduce manual labour and eventually minimise the chances of errors in medical processes. Some common forms of technology used in healthcare other than EHRs include automated IV pumps, portable monitors, wearable devices, telehealth and others.
LO4: Keeping and maintaining records in a care setting in line with national and local policies and appropriate legislation
Effectiveness of documentation completion
Among the different benefits of completing a documentation process, some have even been found to be opined by most health professionals. Firstly, documentation serves as a basis for care continuity for the organisation and will serve as meaningful data in future. As mentioned by Rathee et al. (2020), most professionals have said that documentation has been helpful in risk management and protected them against malpractice lawsuits. Documentation is part of professional discipline, especially in healthcare and adhering to it protects professionals from the risks of lawsuits. Similarly, as said by Cerchione et al. (2023), documentation is required to comply with legal regulations and institutional requirements. Assuring compliance with the requirements of clinical documentation is necessary for every professional. Federal and state governments have listed individual requirements regarding record keeping in hospitals and these regulations are necessary to be followed. Also, quality assurance of medical processes mandates documentation. Besides, professional activities, including processes involved in the assessment of patients, can be recorded with adequate documentation (Sheikh et al., 2021). Some other reasons include differential diagnosis, service planning, clinical decision-making and treatment design that are facilitated by effective documentation. Making results of treatments and every other service and facilitating coordination among professionals involve documentation.
Analysis of record maintenance
Maintenance of records mostly implies keeping them in a standard storage process to avoid breaches in any form. In the given hospital setting, both hard copy and soft copy are relied upon for record keeping of service users. Hence, the methods used in the maintenance of these records are different in each case. As opined by Daly, (2020), lamination would be a priority for paper documents since that would prevent any form of damage. Lamination would waterproof documents, which is crucially important in a hospital setting because no professional can avoid handling liquid substances. The fluids provided to service users might also pose a risk for paper documents for which the primary requirement is lamination. These records would be cupboards that are accessible only to authorised professionals. In the case of electronic documents, a data breach would be a potential risk because they would be stored in secured hard drives in encrypted formats.
Aspects of service management
The main requirement for effective management of records is to ensure that they are secured. In the case of paper documents, the laminated patient information would be stored in cupboards that have passwords in them. Other than hospital authority, these passwords would be officially provided only to the professionals who have been assigned to that case. As mentioned by Nyashanu et al. (2020), paper documents are perishable, and hence they are to be stored in areas that are devoid of risks like accidental fire. In the case of electronic documents, though, the criteria would be different. They would be converted to encrypted formats with the help of cyber professionals who have expertise and reliability. Following that, the encrypted documents would be stored in hard drives that are also equipped with passwords. These passwords similarly would be provided only to professionals allocated to that case and no other professionals would be allowed to handle that data.
References
Provided
Ico, (2018), a. Guide to Data Protection. Available at: https://ico.org.uk/for-organisations/guide-to-data-protection/ [Accessed on 15 February 2023]
Ico, (2018), b. Data sharing code of practice. Available at: https://ico.org.uk/media/for-organisations/data-sharing-a-code-of-practice-1-0.pdf [Accessed on 15 February 2023]
IPSOS MORI (2013). E-readiness in the social care sector for SCIE: Final report. Department of Health (2012) Digital Strategy: Leading the culture change in health and care. Available at: https://www.scie-socialcareonline.org.uk/e-readiness-in-the-social-care-sector-for-scie-final-report/r/a11G000000188vFIAQ [Accessed on 15 February 2023]
Nmc, (2023). The Code. Available at: https://www.nmc.org.uk/standards/code/ [Accessed on 15 February 2023]
Scott B. (2004). Health record and communication practice standards for team-based care. NHS Information Standards Board. Available at: https://anaesthesiaconference.kiev.ua/downloads/healthrec_compractice_2004.pdf [Accessed on 15 February 2023]
Others
Almathami, H.K.Y., Win, K.T. and Vlahu-Gjorgievska, E., (2020). Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review.Journal of medical Internet research,22(2), p.e16407.
Apa, (2023). Record Keeping Guidelines. Available at: https://www.apa.org/practice/guidelines/record-keeping [Accessed on 15 February 2023]
Cave, A., Kurz, X. and Arlett, P., (2019). Real‐world data for regulatory decision making: challenges and possible solutions for Europe.Clinical pharmacology and therapeutics,106(1), p.36.
Cerchione, R., Centobelli, P., Riccio, E., Abbate, S. and Oropallo, E., (2023). Blockchain’s coming to hospital to digitalize healthcare services: Designing a distributed electronic health record ecosystem.Technovation,120, p.102480.
Cqc, (2023). Regulations for service providers and managers. Available at: https://www.cqc.org.uk/guidance-providers/regulations-enforcement/regulations-service-providers-managers [Accessed on 15 February 2023]
Daly, M., (2020). COVID‐19 and care homes in England: What happened and why?.Social Policy & Administration,54(7), pp.985-998.
Hernandez-Boussard, T., Bozkurt, S., Ioannidis, J.P. and Shah, N.H., (2020). MINIMAR (MINimum Information for Medical AI Reporting): developing reporting standards for artificial intelligence in health care.Journal of the American Medical Informatics Association,27(12), pp.2011-2015.
Keshta, I. and Odeh, A., (2021). Security and privacy of electronic health records: Concerns and challenges.Egyptian Informatics Journal,22(2), pp.177-183.
Landes, S.J., McBain, S.A. and Curran, G.M., (2020). Reprint of: an introduction to effectiveness-implementation hybrid designs.Psychiatry research,283, p.112630.
Morris, C., Scott, R.E. and Mars, M., (2021). WhatsApp in clinical practice—the challenges of record keeping and storage. A scoping review.International Journal of Environmental Research and Public Health,18(24), p.13426.
Nyashanu, M., Pfende, F. and Ekpenyong, M., (2020). Exploring the challenges faced by frontline workers in health and social care amid the COVID-19 pandemic: experiences of frontline workers in the English Midlands region, UK.Journal of Interprofessional Care,34(5), pp.655-661.
Rathee, G., Sharma, A., Saini, H., Kumar, R. and Iqbal, R., (2020). A hybrid framework for multimedia data processing in IoT-healthcare using blockchain technology.Multimedia Tools and Applications,79(15-16), pp.9711-9733.
Saripalle, R., Runyan, C. and Russell, M., (2019). Using HL7 FHIR to achieve interoperability in patient health record.Journal of biomedical informatics,94, p.103188.
Scott, R.E., Morris, C. and Mars, M., (2021). Development of a “cellphone stewardship framework”: legal, regulatory, and ethical issues.Telemedicine and e-Health,27(3), pp.316-322.
Sheikh, A., Anderson, M., Albala, S., Casadei, B., Franklin, B.D., Richards, M., Taylor, D., Tibble, H. and Mossialos, E., (2021). Health information technology and digital innovation for national learning health and care systems.The Lancet Digital Health,3(6), pp.e383-e396.
Vaishnavi, V., Suresh, M. and Dutta, P., (2019). A study on the influence of factors associated with organizational readiness for change in healthcare organizations using TISM.Benchmarking: An International Journal.
Vazirani, A.A., O'Donoghue, O., Brindley, D. and Meinert, E., (2019). Implementing blockchains for efficient health care: systematic review.Journal of medical Internet research,21(2), p.e12439.
Zulkipli, F.N., Hussin, N., Yatin, S.F.M. and Ismail, A., (2022). Issues and trends of trusted mobile electronic medical records management for healthcare industry: A review.International Journal of Business and Economy,4(1), pp.50-59.



