- DNI 13 Dental Anatomy & Assessment of Oral Health Workbook
- Evidence requirements
- Relationship to GDC Learning Outcomes:
- Relationship to Dental Standard Knowledge, Skills and Behaviours
- 1. Draw atable of deciduous (primary) and permanent (secondary) dentitions. Include:
- 2. Name the SIX stages of tooth for
- 3. Label the following diagram of a tooth:
- 4. Describe the types and functions of the mineralised tissues and supporting tissues of the tooth.
- 5. Label the muscles/salivary glands and ducts on the following diagram
- 6. Describe the function of salivary glands and state THREE reasons why they are important
- 7. Name the following muscles of mastication:
- 8. Name the following muscles of mastication:
- 9. Draw atable containing the FOUR muscles of mastication andtheirposition ontheskull, i.e., point of insertion andpoint oforigin and action.
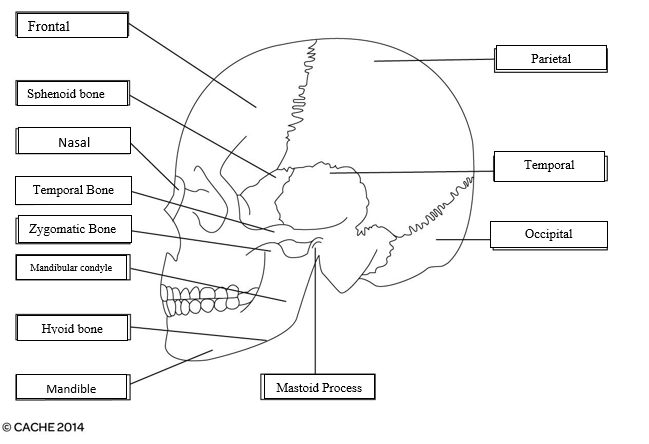
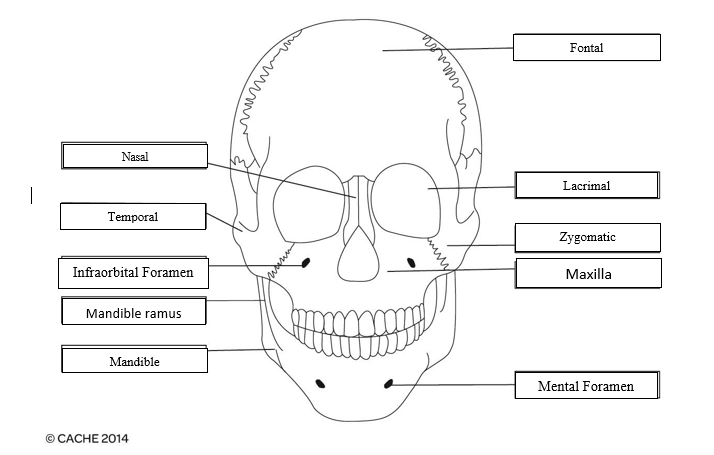
- 10. Label the following diagrams of the skull:
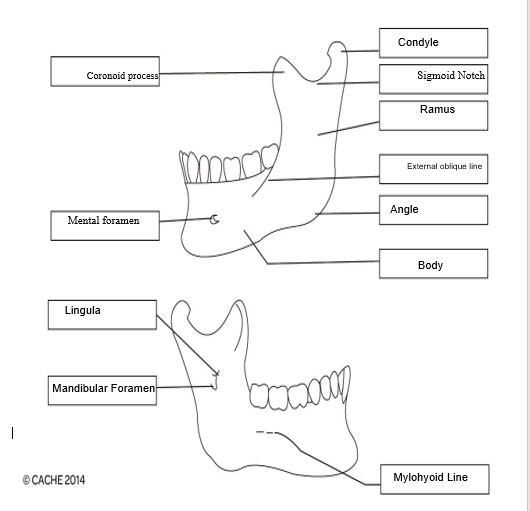
- 11. Identify and label the diagram below:
- 12. Describe the movements of the temporomandibular joint.
- 13. Source and label a diagram that describes the nerves and their branches and the blood supplyto the teethand supporting structures.
- 1. Describe the methods associated with TWO of the following and evaluate:
- 2. Oral assessment is a routine procedure performed in the dental surge Explain TWO of the following:
- 3. Research the General Dental Council (GDC)principle of consent and explain how and why informed/valid consentshould be obtained before any treatmentis undertaken.
- 1. Explain the different classifications of malocclusion
- 2. List four different types of orthodontic appliances used, and briefly explain their role intreatment
- 3. Design a leaflet for a patient due to start orthodontic work. Explain:
- 4. Explain the Dental Nurse’s role when providing support during the different stages of orthodontic assessment and treatment
- 1. Explain FOUR of the following conditions:
- 2. Research and write a short report on how ageing can affect the soft and hard tissues of the mouth.
- 3. Briefly report on how FOUR of the following medical conditions can affect the oral tissues:
- 1. Complete the table below describing the diagnosis, prevention, and management of malignant or potentially malignant lesions:
- 2. Complete the table below giving examples of the named drugs/medications and their use in dentistry
- 3. For three of the following areas, give two examples of diseases and describe their diagnosis and how they are managed:
- 1. Identify FOUR potential medical medical emergencies that could take place in the hospital.
- What have you learnt or how has this reinforced what you already knew?
- What was good about completing this workbook?
- What did you find difficult?
- How will your learning be used in practice?
DNI 13 Dental Anatomy & Assessment of Oral Health Workbook
Introduction
This workbook accompanies the dental anatomy and assessment of oral health sessions delivered by your tutorit will consist of a series of questions and require you to research information.
You will use varying methods to enable you to complete these questions. All can be completed using either written, type or audio answers to demonstrate your knowledge and understanding of how you support your service users within your setting. Discuss with your tutor and decide your preferred method.
This unit has six learning outcomes
The learner will:
- Know the basic structure and function of oral and dental anatomy.
- Understand the methods of dental assessment.
- Know the clinical assessments and instructions associated with orthodontics.
- Understand the changes that may occur in the oral tissues.
- Understanding the management of oral health.
- Know the medical emergencies that may occur in the dental environment.
Evidence requirements
Minimum requirement of one observation. Supporting evidence of learner understanding must be completed and provided in order to support performance evidence. Simulation is allowed for this unit.
- Unit DNI 13: Dental anatomy and assessment of oral health (A/618/4920)
- This unit focuses on knowledge of dental anatomy and oral health with regard to assessment and treatment planning
- Guided learning hours for unit DNI 13 is 29 hours.
- This unit is mandatory and is not graded all criteria must be met before completion of this unit.
- This unit is evidence-based and will provide under pinning knowledge in preparation for your exam at end point assessment.
Relationship to GDC Learning Outcomes:
1.2, 1.1.3, 1.1.5, 1.1.6, 1.1.9, 1.2.1, 1.2.2, 1.2.4, 1.2.5, 1.5.1, 1.5.2, 1.7.2, 1.8.4, 1.9.1, 3.3, 8.1, 12.1
Relationship to Dental Standard Knowledge, Skills and Behaviours
- K25: Know and understand the importance of maintaining accurate and current patient records in accordance with legal and regulatory requirements
- K26: Know and understand the principles of information governance
- K30: Know and understand contributing factors that can impact on oral and general health
- K31: Know and understand a range of conditions that could contribute to medical emergencies
- K32: Know and understand the principles of First aid in the workplace
- K33: Know and understand the regulatory requirements regarding documentation of medical emergencies and first aid incidents
- K34: Know and understand your own competence and limitations in dealing with medical emergencies.
- K5: Know and understand the basic principles of a population healthcare approach including safeguarding, oral and general healthcare and your duty of care
- K6: Know and understand how to raise concerns as described in the current General Dental Council guidance
- K7: Know and understand dental and regional anatomy
- K8: Know and understand the respiratory and circulatory system
Need online assignment help in the UK? Native Assignment Help is your ultimate solution. Our seasoned writers possess the expertise to craft impeccable assignments that meet the highest academic standards, guaranteeing your success.
Task1
(learning outcome 1, assessment criteria 1.1, 1.2,1.3, 1.4,1.5 and 1.6)
1. Draw atable of deciduous (primary) and permanent (secondary) dentitions. Include:
|
Deciduous |
Upper |
Roots/Cusps |
Lower |
Roots/Cusps |
Function |
Age of eruption |
|
“Incisor 1” |
“Incisor 1” |
1½ years |
“Incisor 1” |
1½ years |
The main function is to cut food substances. |
10 months(upper) and 8 months (Lower) |
|
“Incisor 2” |
“Incisor 2” |
2 years |
“Incisor 2” |
1½ years |
It helps to cut the food and also helps to give support to the lips. |
11 months (upper) and 13 months (Lower) |
|
“Canine” |
“Canine” |
3½ years |
“Canine” |
3½ years |
Canine helps to chew the food in mastication. |
19 months (upper) and 20 months (Lower) |
|
“Molar” |
“Molar” |
2½ years |
“Molar” |
2½ years |
It helps to crush and chew the food to swallow and digest the food. |
16 months (upper) and 16 months |
|
“Arch” |
“Maxillary arch” |
3 years |
“Mandibular arch” |
3 years |
It helps in sensation and also in speech. |
29 months(upper) and 27 months |
|
Permanent |
Upper |
Roots/Cusps |
Lower |
Roots/Cusps |
Function |
Age of eruption |
|
“Central incisor” I1 |
I1 |
10 years |
I1 |
9 years |
While taking a bite of food central incisor helps to slice the food substance. |
6-7 years (lower) and 7-8 years (upper) |
|
“Lateral incisor” I2 |
I2 |
11 years |
I2 |
10 years |
It helps to divide the food materials. |
7-8 years (lower) and 8-9 years (upper) |
|
“Canine” C |
C |
13-15 years |
C |
12-14 years |
Guides the teeth for positioning and also maintains the shape of the lips. |
9-10 years (lower) and 11-12 years (upper) |
|
“First premolar” P1 |
P1 |
12-13 years |
P1 |
12-13 years |
During mastication, it helps to tear the food. |
10-12 years (lower) and 10-11 years (upper) |
|
“Second premolar” P2 |
P1 |
12-14 years |
P1 |
13-14 years |
Accommodates the first molar mandibular while mastication. |
11-12 years (lower) and 10-12 years (upper) |
|
“First molar” M1 |
M1 |
9-10 years |
M1 |
9-10 years |
Helps to establish a balance of the blockages. |
6-7 years (lower) and 6-7 years (upper) |
|
“Second molar” M2 |
M2 |
14 to 16 years |
M2 |
14-15 years |
It helps to grind, crush and chew the plant food substances. |
11-13 years (lower) and 12-13 years (upper) |
|
“Third molar” M3 |
M3 |
18-25 years |
M3 |
18-25 years |
It also helps to grind the foods into pieces for easy swallowing. |
17-21 years (lower) and 17- 21 years (upper) |
2. Name the SIX stages of tooth for
|
1. “Initiation stage”: The period of this stage is the sixth to seventh weeks.“Ectomesenchyme cells” gathers instantly below the oral epithelium.Theoral epithelium then multiplies into theEctomesenchyme, which forms a primary epithelial band. |
|
2. “Bud stage”: This stage starts from the eight weeks. The enamel organs are inflamed by dental lamina. From the help of these enamels’ organs evolve each tooth. |
|
3. “Cap stage”: “Middle of the ninth and tenth week”.During the cap stage of tooth development, the cells start to shape the outside layer of the tooth. A cap that formed sits on the tooth bud. Gradually the enamel organ will grow enamel and dental papilla with construct dentin and pulp. |
|
4. “Bell stage”: “Eleventh to the twelfth week”.The bell stage diverges into the “early bell stage” and “late bell stage”. |
|
5. “Apposition stage”: Varies from one tooth to another.The enamel, dentin and cementum are produced in layers. These tissues are primarily secreted as an origin which is particularly calcified. |
|
6. “Maturation stage”: This stage also varies per tooth.The development of the tooth begins when the final tissue density has been deposited. Maturation refers to a primary transitional pre-stage when the morphology and purpose of the organ cells change. |
3. Label the following diagram of a tooth:
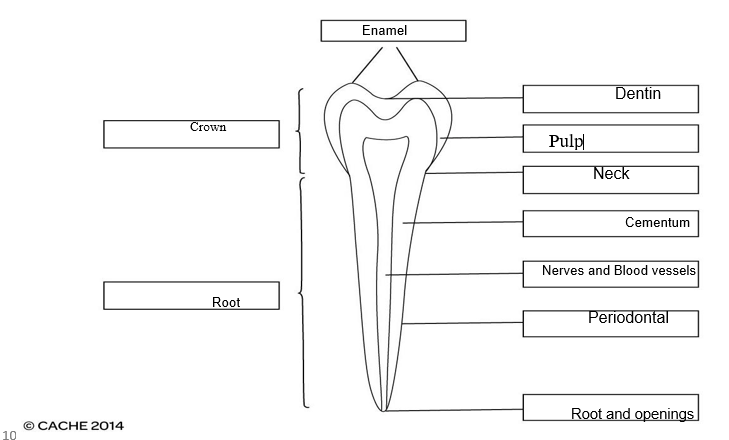
4. Describe the types and functions of the mineralised tissues and supporting tissues of the tooth.
|
Mineralized Tissues: A wide dentin layer forms the majority of “dental mineralized dental tissues”. Mineralized tissues of a tooth contain three different parts includes Dentine, Enamel and Cementum. The main function of Dentine is to give support to the enamel structure. Dentine is also involved in transferring the notions from the enamel to the pulp. Enamel is the hardest matter in the human body and it provides a tough outer layer of the alveolar crown. The primary function of the cementum is to give support to a tooth. Supporting Tissues: The main supporting tissue of a tooth is known as Periodontium. It consists of four components: Alveolar bone, Gingival tissue, Periodontal ligament and cementum. The function of the periodontium is to give support to the tooth, also to guard its microflora and make the attachment between the tooth and bone. Alveolar bones support the teeth throughout the alveoli of each tooth. Gingival tissues give mechanical fencing against bacterial infringement. The major function of the periodontal ligament is to produce the forces of tooth explosion and to supply sensory instruction. |
5. Label the muscles/salivary glands and ducts on the following diagram
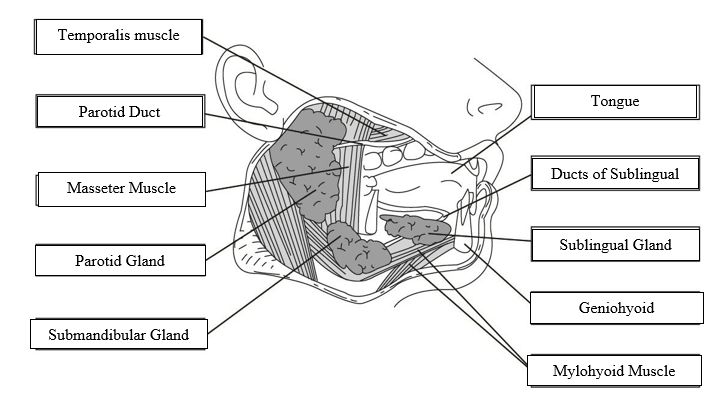
6. Describe the function of salivary glands and state THREE reasons why they are important
|
Saliva is a mixture of digestive enzymes, antibacterial items, water and mucus. Function: Salivary glands have three major parts: Sublingual glands, Submandibular glands, and Parotid Glands. Salivary glands play several roles in the mouth and the digestion of food. One major enzyme named alpha-amylase helps to break down the carbohydrates or starch present in our foods and turns them into simpler forms of glucose and maltose. When a person chews, he/she activates these three glands to emit an enzyme which helps in the food digestive process. Saliva has lubricating effects, which guard inside the mouth cavity, teeth and throat whenever a human body starts to swallow a food bolus. The glans also helps to keep up the ph levels of the mouth. in digestion and also protect teeth against harmful bacterias. Saliva contains several special enzymes that assist in digestion. There is an enzyme named amylase present in saliva which can break down starches into sugars so that the body can easily absorb them. Saliva also helps in cleaning the mouth as well as teeth and tongue. Saliva Contains 99% of Water and also it is an alkaline secretion. The main role of saliva also helps to taste the receptors of the mouth. The parotid gland produces 25-30% of total saliva regularly, which is released by the parotid duct. Only the parotid gland secretes purely aqueous saliva. The submandibular gland releases up to 70% of saliva daily. And the sublingual gland produces 5% saliva regularly. |
|
1. The major importance of the salivary glands is these glands help to make saliva, which plays an important role in food digestion by giving moisture to the food so that the human body can swallow the food easily. |
|
2. Saliva plays another important role in our oral health. Infection in the mouth and throat can be prevented by saliva. Also, saliva is very helpful as it maintains healthy teeth and prevents bad teeth. |
|
3. The salivary contents of the mouth help to maintain and gives protection to the oral mucosa and provide lubrication. |
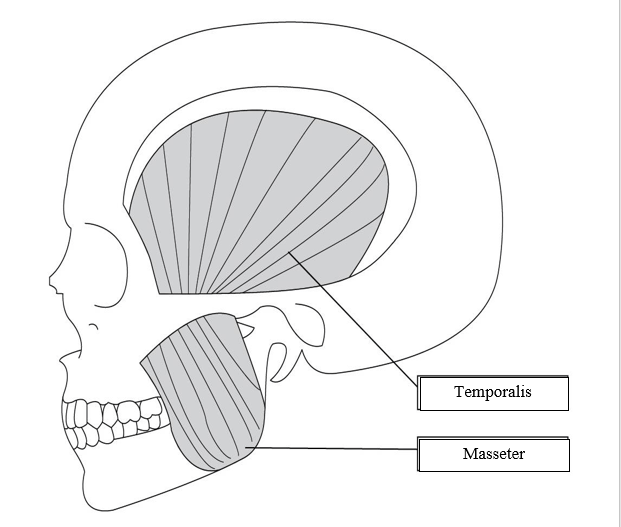
7. Name the following muscles of mastication:
8. Name the following muscles of mastication:
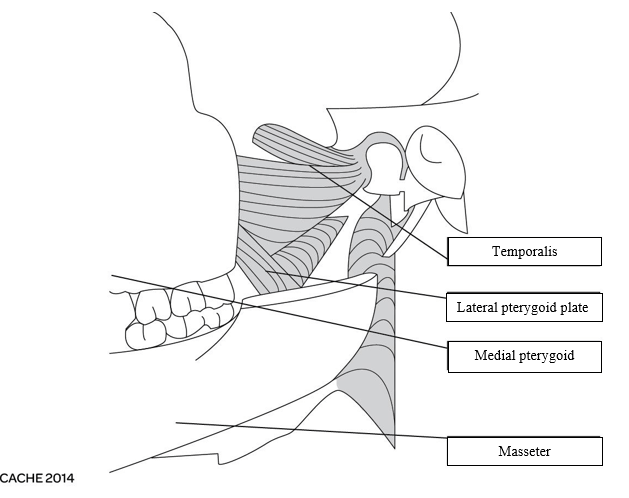
9. Draw atable containing the FOUR muscles of mastication andtheirposition ontheskull, i.e., point of insertion andpoint oforigin and action.
|
1. Temporalis Muscle: Position: “Joins above the bone and fascia in the temporal fossa”. Point of Insertion: In between the process of mandible relies medial on and apex surface Origin: “From the temporal fossa to the inferior temporal line of the lateral skull.” Function: The temporalis muscle’s anterior and mid fibres help to raise the mandible. And posterior fibres help to recant the mandible. |
|
2. Medial Pterygoid: Position: “Present on the medial aspect of the lower jaw”. Point of Insertion: “Medial surface of ramus” and “angle of mandible”. Origin:Arises from the “medial surface” to the “lateral pterygoid plate” of the “sphenoid bone.” Function: To maintain the elevation and swelling of the mandible. |
|
3. “Lateral Pterygoid”: Position: “Located deep to the temporalis and masseter muscle”. Point of Insertion: Adjacent to the “articular disc” and “fibrous capsule” of the “temporomandibular joint”. Origin: Upper head comes out from the “inferior temporal surface” and the Lower head arises from the “lateral aspect” of the “lateral pterygoid gland”. Function: It functions as the major “muscle of mastication” which causes dejection of the mandible. |
|
4. Masseter: Position: “From cheekbone to jaw”. Point of Insertion: “lateral surface and angle of ramus of mandible”. Origin: “inferior zygomatic arch and the two-thirds of the anterior zygomatic arch". Function: Retreat and obtrude the mandible. |
10. Label the following diagrams of the skull:
11. Identify and label the diagram below:
12. Describe the movements of the temporomandibular joint.
|
The major function of the temporomandibular joint is to smoothen the movements of the lower jaw. The movements are divided into two parts: Transitional movement and rotational movement. Rotational movement happens within the “inferior cavity” of the joint. Transitional movement mediates between “Lateral pterygoid, medial pterygoid muscle, masseter”. Temporomandibular joints can be described as lateral deviation protrusion and retrusion as well elevation of mandible and depression. It acts as hinge which facilitates the closing and opening of the mouth. Additionally, sliding motion is also regulated by this joint. |
13. Source and label a diagram that describes the nerves and their branches and the blood supplyto the teethand supporting structures.
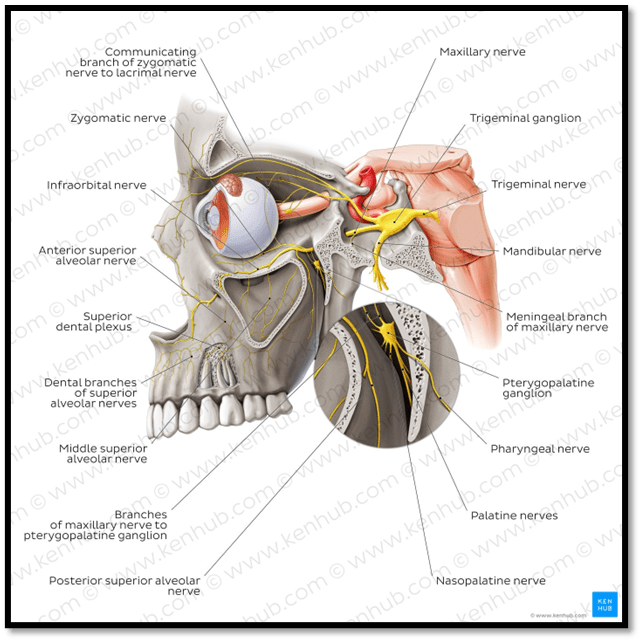
Kenhub, 2022
Task2
(Learning outcome 2, assessment criteria2.1, 2.2,2.3, 2.4,2.5,2.6and2.7)
1. Describe the methods associated with TWO of the following and evaluate:
Assessing and recording soft and hard tissue
Assessing and recording of periodontal conditions
Measuring pulp vitality
|
● Assessing and recording the hard tissues are necessary for a complete check of the dental cavity. The assessment includes Leakage, Decay, Positioning, Impactions and necessary treatment. Both the dentine and the enamel should be reviewed. Soft tissue oral assessment is a little bit more complicated than hard tissue examination; it involves the mouth, gums, throat, tongue, lips, cheeks and floor of the mouth. ● Periodontal assessment is necessary which involves the recording of a full mouth examination and to take the bleeding data also tooth potency, and downturn also is the major parameters. Periodontal assessment is necessary for the identification of the at risk patients who exceptionally required dental care. |
2. Oral assessment is a routine procedure performed in the dental surge Explain TWO of the following:
- The main purpose of an oral health assessment
- The reasons for taking photographs and radiographs when diagnosing and treatment planning
- What materials are used during an oral health assessment and why
|
● The main reason for an oral health assessment is to make sure dental health in long term. Regular oral health assessment helps to get rid of mouth cancer and gum disease. Also, good oral health can be maintained, bad teething can be prevented. Oral health assessment is essential from restorative approach perspective. It helps in prevention of early tooth decay, loss of tooth as well as identification of the prevalent disease. ● Dental x ray is important for produce an image in order to plan correct treatment. With help of radiographs dentist can view the condition of roots, facial bones and jaw placement. Primary aim of doing dental photography is to record extra and intra oral manifestations. It facilitate in improvement of the quality of dental care as well as helps in keeping a track of status of important dental practices. ● The main materials, which are used in oral health assessment, include Toothbrushes and fluff, Scrapers of the tongue, mouth irrigators and Mouthwash. The everyday uses of Toothbrushes and fluff help to prevent cavities, periodontal diseases, enamel weakening, and tooth loss. Scrapers of the tongue help to remove oral bacteria, total immunity can be boosted and saliva production can be promoted. Mouth irrigators help to freshen breath, gum health will improve and the main function of a Mouthwash is to prevent bad breathing. |
3. Research the General Dental Council (GDC)principle of consent and explain how and why informed/valid consentshould be obtained before any treatmentis undertaken.
|
There are 9 major principles for “General Dental Council (GDC)” such as: Listening to the patient’s interests, and preferences and treating them in a safe and clean environment. Communication should be effective with every patient to gather the full information about their problems. A patient’s consent is valuable. A patient’s information should be maintained and protected. Their complaints should be assessed promptly. The whole dental care team should work as a good team to gain the interest of a patient. Work should be developed with professional skills and pieces of knowledge. If a patient’s health is at risk, the doctor should raise immediate concerns. A doctor should keep in mind that a patient’s interest can be developed by the good behaviour of a doctor. Dental consent is essential to avoid the legal issues which can happen during treatment of dental practice. Additionally it helps in processing rights of the patients during whole dental treatment procedure. |
Task3
(Learning outcome 3, assessment criteria 3.1, 3.2, 3.3 and 3.4)
1. Explain the different classifications of malocclusion
|
According to the study, it has been found that there are mainly three types of malocclusions Type 1: In type 1 malocclusion, the alignment of the teeth is good, but the shape of the arch is quite abnormal. Type 2: In type 2 malocclusion, the alignment of the upper front teeth is fine, but the lower front teeth are leaned towards the tongue (Issraniet al., 2022). Type 3: In type 3 malocclusion, the arch of the upper teeth is underdeveloped and that is why the lower teeth have good alignment. |
2. List four different types of orthodontic appliances used, and briefly explain their role intreatment
|
1. Elastics |
It often helps in improving the fitness of the lower and upper teeth (Mohammed et al., 2021). Elastics are used in the correction of a misaligned jaw. This works to make conjugation in braces to apply a tender continual force to pull the teeth into alignment. |
|
2. Forsus |
“Forsus Fatigue Resistant Device” can be defined as the alternative headgear that helps in promoting the growth of adolescents. In addition, it often helps in eliminating the rate of excessive overbites by improving the fitness of the teeth. |
|
3. Headgear |
Headgear is used in treating the overbite of the upper jaw which is forwarded to the lower jaw. Headgear is frequently used to correct malocclusions means when there is misalignment between the maxilla and mandible. |
|
4. Palatal Expander |
It helps to expand the upper jaw with the help of gentler pressure on the upper molars. Palate expanders give the dentist more space to move the teeth around to overlapping and other oral problems. This tool is most common in children. |
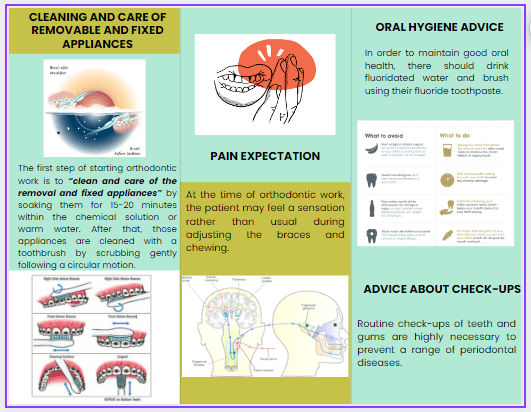
3. Design a leaflet for a patient due to start orthodontic work. Explain:
- Cleaning and care of removable and fixed appliances
- What to expect (pain,other)
- Oral hygiene advice and advice about check-ups,etc.
- The first step of starting orthodontic work is to “clean and care of the removal and fixed appliances” by soaking them for 15-20 minutes with the chemical solution or warm water. After that, those appliances are cleaned with a toothbrush by scrubbing gently following a circular motion.
- At the time of orthodontic work, the patient may feel a sensation rather than usual during adjusting the braces and chewing.
- In order to maintain good oral health, there should drink fluoridated water and brush using their fluoride toothpaste. Routine check-ups of teeth and gums are highly necessary to prevent a range of periodontal diseases.
4. Explain the Dental Nurse’s role when providing support during the different stages of orthodontic assessment and treatment
|
The primary role of the dental nurse is to ensure that, all the necessary materials, as well as the instruments, have been set properly before starting any treatment procedure. On the other hand, the nurse helps to follow the cleaning procedure after the post-operatic time (Abatiet al., 2020). Moreover, the dental nurse also helps the patient by supporting the system of fixed appliances. That is how the dental assistant often helps in all the clinical procedures during and after the dental treatment. |
Task4
(learning outcome 4, assessment criteria4.1, 4.2and 4.3)
1. Explain FOUR of the following conditions:
- Oral cancer
- Lichen planus
- Oral candidiasis
- Herpes simplextype1
- Glossitis
- Osteoporosis
- Salivary gland disorders (xerostomia)
|
1. Oral Cancer: This often appears like a growth within the mouth. Primary symptoms of oral cancer are Swelling/thickenings, lumps or bumps, and rough spots. Oral cancer affects the mouth. It looks like a normal problem in the lips or mouth, it can appear like white patches that bleed. This type of cancer can spread throughout the mouth as well as the throat. |
|
2. Lichen planus: Due to swelling and irritation in the skin, hair, and nails as well as mucous membrane, there often arise this kind of condition in the human body. Lichen planus can trunks up as white, lacy patches, open sores or red and swollen tissues. This disease needs regular monitoring because they can develop mouth cancer at any point in time. |
|
3. Oral candidiasis: This kind of condition often arises within the mouth due to the growth of the fungus Candida albicans in the lining of the mouth.The sign and symptoms of oral candidiasis include creamy white discharges on the inner cheeks and tongs and sometimes in the gums and tonsils. It is a conciliatory infection of the oral cavity. |
|
4. Herpes simplex type 1: The infection that is caused by the herpes simplex virus (HSV) is often known as herpes and is transmitted by oral contact and creates infections in the mouth. Herpes simplex type 1 affects lips, mouth or gums. The symptoms are small and painful blisters which are called fever blisters. This is responsible for setting up initial and repeated vesicular discharge. |
2. Research and write a short report on how ageing can affect the soft and hard tissues of the mouth.
Ageing can be effective for the older ones, but that can badly affect the gums and that is why the gums can become thinner and reduces their normal density (Ghorbanyjavadpouret al., 2019). In addition, ageing can create cavities within the root of the teeth due to the accumulation of bacteria, which causes the decay of the teeth. These kinds of symptoms are quite normal for people of the age group over 45 and often arise in both males and females.
3. Briefly report on how FOUR of the following medical conditions can affect the oral tissues:
- Oral cancer
- Herpes simplextype1
- HIV
- Hepatitis B
- Diabetes type 2
- Epilepsy
- Eating and digestive disorders
|
1. Oral Cancer: This kind of disease often causes pain in different ways. In this disease, there often arises tumour, that badly affects the nerves of the oral cavity and causes inflammation. |
|
2. Herpes simplex type 1: It often causes damage to the soft tissue of the gums and the entire oral cavity. For this reason, the gums and teeth have been separated and there grow bacteria in the cavity. |
|
3. HIV: According to a study by (NIH, 2022), it has been found that HIV is too effective for the patient, which causes "chronic dry mouth, gingivitis, bone loss around the teeth, canker sores, oral warts, fever blisters, oral candidiasis” and so on. |
|
4. Hepatitis B: This virus often creates manifestation in the oral cavity, which can cause oral cancers in the presence of these symptoms such as "lichen planus, Sjögren's syndrome, and sialadenitis”. |
Task5
(Learning outcome 5, assessment criteria 5.1, 5.2, 5.3 and 5.4)
1. Complete the table below describing the diagnosis, prevention, and management of malignant or potentially malignant lesions:
|
Methods of diagnosis |
Prevention |
Management |
|
|
Malignant lesions |
In order to diagnose the malignant lesions, doctors need to do a biopsy of the oral tissue. Imaging tests using the “computerized tomography (CT)scan”, “positron emission tomography (PET) scan”, and “ultrasound and X-ray” (Cicciù, et al.,2019)techniques can be helpful to identify the types of cancer. |
For the prevention of malignant lesions, there use to stop the use of tobacco and should take a healthy diet. Following a healthy body weight and regular medical care are essential for the prevention of malignancy. |
“Medical treatments such as chemotherapy, radiation or targeted drug therapy, to surgical treatments” can be the range of options for managing malignant lesions. |
|
Potentially malignant lesions |
VELscope is known as the diagnostic device for identifying the presence of potentially malignant lesions that is present in the oral mucosa. |
Immunotherapy is a potential method for the prevention of potentially malignant lesions. |
In order to manage this kind of lesion there should focus on “riskmodification, surveillance, symptom management and directed biopsies”. |
2. Complete the table below giving examples of the named drugs/medications and their use in dentistry
|
Drugs/Medications |
Example |
Use in dentistry |
|
Analgesics |
Acetylsalicylic Acid (Aspirin) Hydrocodone |
It is used in dentistry for reducing the pain of the teeth and also it can be effective in preventing (Dar-Odeh et al., 2019) side effects like fever It is utilised as a medicine for hurtful tooth diseases. |
|
Antibiotics |
Amoxicillin |
The use of this antibiotic in dentistry often helps in preventing dental infections. It is used to prevent dental infections after “surgical interventions” such as pulp debridement, incision and drainage |
|
Anti-Viral |
Acyclovir |
This kind of antiviral drug is effective to prevent viral infections like Herpes simplex infection in the teeth. It is utilised to treat infections induced by specific kinds of viruses. |
|
Anti-fungal |
fluconazole polyenes |
It is used to treat oral infection by the fungus. Secure with “ergosterol” in the “fungal cells” and create voids, inducing cell demise because of the the leaking out of the cell ranges |
|
Tranquilisers/hypnotics |
triazolam (Halcion) Zaleplon |
This kind of drug is used for the sedation of the oral cavity. This drug is known as hypotonic and helps to get sleep faster. |
|
Emergency drugs |
Epinephrine Nitroglycerin |
It is helpful in dentistry “to numb the mouth before a dental procedure”. Helps to prevent chest pain, and it is also used to get relief from an “angina attack”. |
3. For three of the following areas, give two examples of diseases and describe their diagnosis and how they are managed:
- The oral mucosa
- Soft tissue
- Facial pain
- Facial bones
- Facial joint
- Salivaryglands
|
Diagnosis |
Two examples |
Diagnosis/managed |
|
1. The oral mucosa |
1. Oral lichen planus 2. Stomatitis |
1. Oral Lichen Planus can be diagnosed with the help of a Biopsy, blood culture and blood tests method. 2. Stomatitis can be diagnosed with the help of a physical examination “to identify the severity of pain and the presence of triggers”. |
|
2. Soft Tissue |
1. gastroesophageal reflux disease 2. hematoma |
1. It can prevent by maintaining proper healthy teeth. 2. Practising good oral hygiene e is the best option to prevent the secretion of blood from teeth. |
|
3. Facial Pain |
1. Trigeminal neuralgia 2. Myofascial pain syndrome |
1. With the help of anticonvulsants, it can be minimized. 2. Improvement of the posture can hello the patient get relief from myofascial pain. |
Task6
(learning outcome 6, assessment criterion6.1)
1. Identify FOUR potential medical medical emergencies that could take place in the hospital.
|
1. Cardio-respiratory arrest: It is also called cardiopulmonary arrest due to the cessation of the function of the heart and the respiratory system, which causes sudden death. A cardio-respiratory arrest can happen when a patient is treated with an anaesthetic. It also can happen when accurate emergency care is not given to a patient who is under dental surgery. |
|
2. Anaphylactic shock: Anaphylactic shock is a major and life-threatening allergic reaction which can occur in dental surgery.This often arises due to the release of foods as well as chemicals that causes a drop-down in the blood pressure for block breathing and narrowing the airways. |
|
3. Epilepsy: During any dental surgery, the brain may perform activities abnormally that cause a sensation in the body. |
|
4. Hypoglycemia: At the time of dental surgery, blood sugar may fall below 3 mmol per litre., which causes sweating & fatigue. Hypoglycaemia is one of the most dangerous during the perioperative period. Acute hypoglycaemia can result in brain injury permanently. |
For further tasks on medical emergencies and meeting assessment criteria 6.2, please refer to those in unit UFAEI: Firstaid essentials, which can be cross-referenced.
Learner declaration of authenticity: DNI13
I declare that the work presented for this unit/task is entirely my own work.
Learner signature: Date:
For e-portfolio a signature is not required, providing the learner has a personalised and secure login.
REFLECTIVE ACCOUNT
Think about what you have learnt during this unit. How has your knowledge improved and how have you applied this to your working practice? Please reflect below on the workbook you have completed by answering the following questions.
What have you learnt or how has this reinforced what you already knew?
|
Conducting this study, helped me learn the proper use of the necessary appliances in dental practices. Moreover, this study has helped me to know the appropriate use of emergency drugs during dental surgery. |
What was good about completing this workbook?
|
Completion of this workbook has helped me to gather in-depth knowledge about the disease due to unhygienic dental practices. Moreover, throughout this study. I have understood that a person must need to take care of their oral that can prevent future risks related to oral cancer, herpes and so on. In addition, I learnt that the person having HIV, or diabetes, must need to be more careful about their oral health, which may prevent the infection of the soft tissue. |
What did you find difficult?
|
After completing this study, I have analyzed, during dental surgery of the emergency medication situations like anaphylaxis, and epilepsy, cardio-respiratory arrest, a haematoma can be more effective for the patient. For instance, the amount of rising amount of Adrenaline can cause an increment in sugar level that triggers the rate of hypoglycemia during dental surgery. |
How will your learning be used in practice?
|
Learning through this assignment, I have gathered various kinds of relevant knowledge based on the subjects, that can be helpful for me in my future workplace. Especially, the knowledge of medications based on the emergency medication situation will be advantageous for me during taking any methods to diagnose the dental related diseases in the patient. Moreover, this study was helpful in learning the appropriate use of essential tools and techniques. |
|
How long has it taken you to complete this workbook? |
HRS |
MINS |
Reference List
Journals
- Abati, S., Bramati, C., Bondi, S., Lissoni, A. and Trimarchi, M., 2020. Oral cancer and precancer: A narrative review on the relevance of early diagnosis. International journal of environmental research and public health, 17(24), p.9160.
- Cicciù, M., Cervino, G., Fiorillo, L., D’Amico, C., Oteri, G., Troiano, G., Zhurakivska, K., Lo Muzio, L., Herford, A.S., Crimi, S. and Bianchi, A., 2019. Early diagnosis on oral and potentially oral malignant lesions: a systematic review on the VELscope® fluorescence method. Dentistry Journal, 7(3), p.93.
- Dar-Odeh, N., Babkair, H., Abu-Hammad, S., Borzangy, S., Abu-Hammad, A. and Abu-Hammad, O., 2020. COVID-19: present and future challenges for the dental practice. International journal of environmental research and public health, 17(9), p.3151.
- Ghorbanyjavadpour, F. and Rakhshan, V., 2019. Factors associated with the beauty of soft-tissue profile. American Journal of Orthodontics and Dentofacial Orthopedics, 155(6), pp.832-843.
- Issrani, R., Prabhu, N., Siddanna, S., Alanazi, S.H., Alam, M.K., Munisekhar, M.S., Hamza, M.O., Shabanah, R.F.D. and Gadh, R.S.A., 2022. Cone Beam Computerized Tomographic Analysis of Collum Angle of the Maxillary Central Incisors in Different Types of Malocclusion: Comparative Assessment in Saudi, Jordan and Egypt Subpopulation. Diagnostics, 12(6), p.1506.
- Kim, M.G. and Park, C.H., 2020. Tooth-supporting hard tissue regeneration using biopolymeric material fabrication strategies. Molecules, 25(20), p.4802.
- Könönen, E., Gursoy, M. and Gursoy, U.K., 2019. Periodontitis: a multifaceted disease of tooth-supporting tissues. Journal of clinical medicine, 8(8), p.1135.
- Mohammed, M., RAHMAN, N.A. and Samsudin, A.H.Z., 2021. The Impact of Different Types of Orthodontic Appliances and Its Location in Producing CT Scan Artefacts. Sains Malaysiana, 50(10), pp.3067-3075.
- Fatima, S., Muzammal, M., Rehman, A., Shah, K.U., Kamran, M., Mashal, S., Rustam, S.A., Sabir, M.W. and Nayab, A., 2020. Composition and function of saliva: A review. Wordl Journal of Pharmacy and Pharmaceutical Sciences, 9(6), pp.1552-1567.
- Miyaoka, Y., 2019. Quantitative Analysis of Activity Patterns in the Muscles of Mastication and Deglutition. In Voice and Swallowing Disorders. IntechOpen.
- Nickel, J.C., Iwasaki, L.R., Gonzalez, Y.M., Gallo, L.M. and Yao, H., 2018. Mechanobehavior and ontogenesis of the temporomandibular joint. Journal of dental research, 97(11), pp.1185-1192.
- Kossioni, A.E., Hajto-Bryk, J., Janssens, B., Maggi, S., Marchini, L., McKenna, G., Müller, F., Petrovic, M., Roller-Wirnsberger, R.E., Schimmel, M. and van der Putten, G.J., 2018. Practical guidelines for physicians in promoting oral health in frail older adults. Journal of the American Medical Directors Association, 19(12), pp.1039-1046.


