Health & Social Care Policy Ethics and Law Assignment
This assignment critically examines ethical dilemmas, mental capacity, and legal responsibilities in Health and Social Care, focusing on policy application, professional decision-making, and safeguarding vulnerable individuals.
Ph.D. Experts For Best Assistance
Plagiarism Free Content
AI Free Content
Introduction
The policies, ethics, and laws of health and social care form the foundation of professional practice. They ensure that service users receive care that is ethical, legal, and aligned with best practices. This portfolio will address complex dilemmas within the healthcare setting when we apply these principles and when we make decisions that inevitably affect the intersection of competing interests, legal obligations, and ethical considerations. This portfolio critically explores the meeting place of policy, ethics, and law within HSC professional practice and the implications for professional decision-making and responsibility.
The Health and Social Care (HSC) Act's fast-approaching 10-year anniversary serves as an opportune time to dissect its underpinnings, renewels, and sometimes regressions. HSC's increasingly fragile edifice (appearing in successive Conservative and New Labour editions) reflects an increasingly adverse atmosphere in which even the most severely disabled expect, and in fact, deserve, `enhanced protections for vulnerable individuals. This portfolio will look at a particular ethical quandary plaguing HSC, charting its course through history in an annotated timeline (The King's Fund, 2022). The portfolio will then place the timeline's events in the context of our current legal and policy environment. It will consider not just the particular legalities and policies at play but also the broader ethical and practical challenges that HSC and other organizations like it face in today's world. At the end of the portfolio's executive summary, the reader will find an assessment of the situation (Health and Care Professions Council., 2025). The portfolio will offer not just an indictment of the current scenario but also recommendations for ameliorating it. This portfolio is an attempt to paint a chiaroscuro of a very important and very contemporary ethical problem.
Part 1: Ethical dilemma
Introduction of the chosen ethical dilemma
Mental capacity
Mental capacity is considered to be the capability to analyze a situation, the consequences of a decision and the options available and to utilize that understanding to make an informed choice. Evaluating and admiring mental capacity presents multifaceted ethical dilemmas within HSC since it requires harmonizing autonomy with the requirement for protection (Wies, Landers & Ienca, 2021). It is stated specifically for those people who may not be able to make knowledgeable decisions, while complying with the legal frameworks like the Mental Capacity Act.

Figure: Mental capacity
In this the key considerations are as follows:
Autonomy vs. Protection: The major conflict lies into admiring the right of an individual in order to make their own decisions even though those decisions might be apparent as harmful or unwise, versus the responsibility to protect people who lack the ability from possible harm.
Best interests: When a person lacks capability, decisions should be made into their best interests (Jokinen, Stolt & Suhonen, 2021). Interpreting and defining best interests could be contested and subjective, resulting into ethical challenges.
Legal frameworks: The Mental Capacity Act 2005, serves a legal framework for evaluating and admiring capacity, but it also enables for interventions like raising ethical questions and deprivation of freedom under particular situations about the degree and the nature of these interventions.
Evaluating capacity: Considering whether an individual lacks the ability to make specific decisions could be multifaceted and needs a detailed assessment that is determined to be challenging for healthcare providers.
Informed consent: Assuring that people who are capable could serve informed consent to interventions or treatment is significant, but in most of the situations this may be impractical or complex (Lewis & Green, 2021).
Advance decisions: Admiring people progress decisions (such as denying treatment) is important but could also generate ethical dilemmas, especially if the person develops a certain condition later, which needs treatment which they refused beforehand.
Proxy decision-making: The act introduces the idea of proxy decision-makers who make choices on behalf of the person who lack the ability, but there comprises of concerns regarding excessive influence and possible conflicts (Martinez-Martin et al., 2021).
Mental Health Act: This particular act is appropriate only while treating a person with mental disorder and it is not always valid while treating a person with physical illnesses that could generate further intricacy.
Part 2: Wider evidence and facts
Mental assessment plays a crucial role in healthcare, most importantly for the elderly, as it directly impacts one’s autonomy, treatment decisions, and that person’s overall welfare. Profound implications for older people’s assessment or inability to assess could result from inadequate assessment or unresolved issues of mental capacity (Gan et al., 2023).
Prevalence of Cognitive Impairments in the Elderly
Older adults are prone to having cognitive impairments, including delirium and dementia. “About 14 percent of adults 60” and over have a mental disorder; depression and anxiety are the most common. These conditions are responsible for “10.6 percent of the years lived with disability in this age group” (World, 2023). It is also worth noting that almost a quarter of people who die by suicide (27.2%) are 60 or over.
Impact on Healthcare Outcomes
The mental issues of capacity can be left unresolved, and these can lead to very adverse effects.
Mortality and morbidity: Elder abuse victims have a three times increased risk of death than nonvictims. Drug begins to affect their brain function, their fingers begin to curl, and then they are physically unable to clean themselves.
Prolonged Hospitalization and Institutionalization: Seniors with cognitive deficits are prone to stay in a hospital longer and then become institutionalized (Gentsch & Kuehn, 2022). Delirium is linked to higher risk of death, longer hospital stays, and the odds of being discharged to a facility other than home.
Challenges in Advance Care Planning (ACP): a required process of aligning medical interventions to a patient’s preference is an imperfect endeavor that is hampered by cognitive impairments (Gan et al., 2023). ACP can help ease patients’ and families’ end-of-life stress, but few elderly use such plans, sometimes because people aren’t aware or given direction.
Systemic Challenges
However, the current healthcare system is not resolved to dealing with cognitively impaired elderly patients' needs systemically.
Lack of Assessment & Oversight: Comprehensive geriatric assessment is needed to assess many relevant aspects of an elderly patient’s health, e.g. cognition, mobility, nutrition, and emotional status (Reynolds et al., 2022). Such assessments help in taking an informed decision about the treatment option considering risks and benefits to best fit in that patient's situation.
Barriers to Continuing Healthcare (CHC): An inherent drawback of the current system that prioritizes financial over genuine healthcare need puts elderly patients with cognitive impairments at a disadvantage in being able to receive adequate support.
Part 3: Annotated timeline
The evolution of the mental capacity policy in the UK was an outcome of a dynamic interplay between the changes in the attitude of the society, the reforms in the laws, and the advancement in the medical understanding.
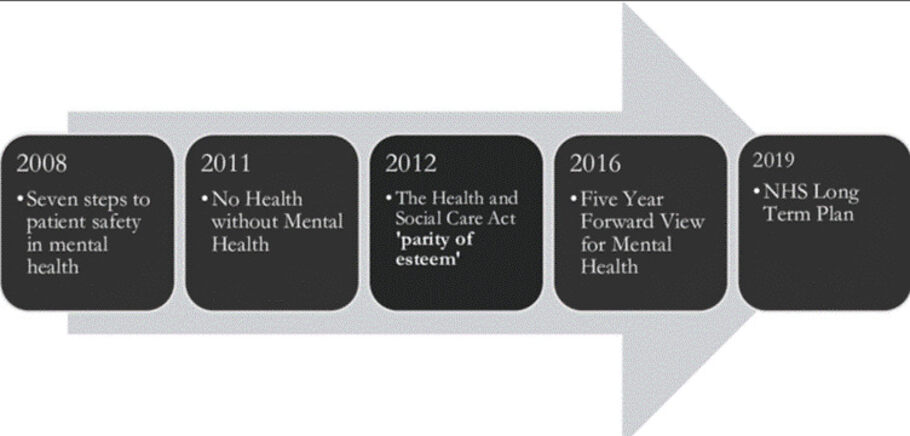
Figure: History of mental capacity policy
1774: Madhouses Act
This was the first UK legislation dealing with mental health, to regulate privately funded lunatic asylums to stop the abuse of individuals with mental disorder.
1845: Lunacy Act and County Asylums Act
These provided for county asylums and the placing of the power to oversee them in a Lunacy Commission and provided for standardized care for persons suffering from mental illness (Caringforcare.co.uk, 2024).
1890: Lunacy Act
It established "reception orders" to formally admit individuals into asylums that had to be reviewed judicially to protect patients' rights.
1959: Mental Health Act
This aimed to give informal treatment to most people with mental disorders and to integrate mental health services into the National Health Service (NHS) as part of the shift towards community care.
1983: Mental Health Act
Laid down a legal framework for the detention and treatment of people, including permissions regarding treatment without the consent of the individual under certain circumstances (Caringforcare.co.uk, 2024).
2005: Mental Capacity Act
It provided a holistic framework of approach to assess mental capacity and make choices on behalf of a person without capacity, and its impetus included empowerment and protection. Protection of human rights, autonomy and obligation to deal with ethical issues in healthcare and social care services (Kirkbride et al., 2024).
2024: Proposed Reforms to the Mental Health Act
The UK government announced a bill to change the approach to treatment for people with autism and learning disabilities, banning the use of prison cells for people in mental health crises and preventing detention under the “Mental Health Act” for those with autism and learning disabilities.
Factors Influencing Policy Development
Policy Changes: The evolution of social attitudes about mental illness from viewing the person as a societal threat to respecting the person’s rights and autonomy had a great impact in policymaking (McDaid et al., 2022).
Legislative Reforms: Legislative reforms were brought about due to improved understanding of mental health conditions, which have risen to advanced levels of medical advancements.
Human Rights Movements: Advocacy for human rights of mentally disordered individuals has led to policies oriented towards empowerment and protection of the rights of individuals, concerning ethical considerations in care (Kirkbride et al., 2024).
Part 4: Components of policy and legal framework and or statutory guidance
Healthcare and social care (HSC) operate in a structured policy and legal framework designed to ensure the safety, rights, and well-being of individuals while maintaining professional standards. These frameworks comprise statutory guidance, regulatory bodies, ethical principles, and procedural safeguards. Collectively, they influence decision-making in HSC. Of course, the reverse is true as well: Decision-making within HSC frameworks influences societal decisions about what constitutes right and wrong in the care of individuals.
1. Legal Frameworks in Health and Social Care
The legal bases for HSC practice exist in national and international laws. In the UK, a landmark piece of legislation is the Health and Social Care Act 2012, which restructured the National Health Service, emphasizing patient-centered care. Also, the Care Act 2014 established a statutory framework for adult social care, emphasizing safeguarding, caretakers' rights, and person-centered planning.
Other vital laws encompass:
The 2010 Equality Act: Makes certain that people cannot be discriminated against when receiving healthcare services. Ensures that people cannot be discriminated against because of their race, gender, or disability, or for any of a number of other specified reasons.
The Mental Capacity Act 2005: Supplies a legal framework for making decisions on behalf of people who cannot make those decisions themselves, and ensures that the rights and best interests of those people are upheld.
The Children Act 1989 and 2004: Sets forth the legal foundation for the welfare of children and safeguarding them, ensuring that the top priority in care services is the welfare of minors.
These legal frameworks are supplemented by the case law, in which judicial decisions further refine and elucidate statutory provisions.
2. Statutory Guidance and Regulatory Bodies
Even though CMS and FDA govern diverse factors of healthcare, FDA governs the utilization and marketing of the medical goods. The mental health care providers are responsible to the statutory bodies. All the mental health practitioners (MHPs) such as the psychiatric social workers, mental health nurses and clinical psychologists along with every MHE will have to be registered with this particular authority (Martinez-Martin et al., 2021). The statutory bodies puts their efforts to make sure that the rights, dignity along with the respect of the mentally ill individuals are uphold while they are under treatment.
Part 5: Exploring key ethical and practical challenges
The MCA 2005 was implemented to safeguard those who cannot make decisions while guaranteeing autonomy. However, the law has, to date, proved to be an ineffective tool in the hands of practitioners owing to its many ethical and practical obstacles. The MCA is built on principles including presuming capacity unless proven otherwise, providing the right support so that people can make decisions, and always putting the person's interests first (Bifarin & Stonehouse, 2021). The purpose of these principles is to achieve a balance between the values of autonomy and protection. Nevertheless, implementation is complex in practice.
Another major challenge is the Deprivation of Liberty Safeguards (DoLS) introduced to prevent unlawful restriction of those who are not able to make decisions for themselves. DoLS is intended to protect vulnerable people but it has been strongly criticised for being too bureaucratic and inconsistent in application. Those cases that do happen, often see delays and endanger people (Lewis, 2021). These concerns were addressed through the introduction of the “Liberty Protection Safeguards (LPS) in 2019”, but time spent working under a floundering system will continue.
Challenges in Implementing Policy
Assessing Mental Capacity: This is a subjective process and there may be differences between the assessment of mental capacity for an individual in any given moment. Inconsistent decisions due to the presence of biases and a lack of clarity (Bifarin & Stonehouse, 2021).
Balancing Autonomy and Safety: Practitioners are left with ethical dilemmas in balancing autonomy with putting the runner’s safety at risk while making unwise decisions.
Insufficient time and staffing: Many social and health care systems are underfunded and lack the time or staffing to perform proper capacity assessments and well-informed best interest decisions (Ruck et al., 2023).
Inconsistent Applications: Professionals working through the outdated and inefficient procedures surrounding implementation of DoLS with LPS still pending must operate under legal risks.
Inadequate Training and Awareness: Due to lack of training and awareness, not all HT staff are trained in the MCA principles, and then misinterpret and wrongly apply the principles (Lewis, 2021).
Ethical Issues: Assisted dying and debates around personal freedoms present additional layers of complexity that force grappling with balancing legal duties with changing and evolving societal perspectives.
Part 6: Recommendations for best practice in applying policy or legislation
It is highly recommended that in order to best apply policy and legislation for mental health disorders, the emphasis must be on the protection of human rights, implementing an inclusive strategy surrounding community incorporation, rehabilitation and treatment (Chieze et al., 2021). This must also involve minimizing disgrace and promoting access to care. The best practices and key elements which must be included are given below:
Human rights focus: The focus must be towards making sure that the legislation and the policies are aligned with global human rights standards, promoting dignity, involuntary treatment along with protecting against abuse.
Access to care: It is strongly recommended to promote access to evidence-based, quality and affordable mental health services which involves making sure equitable access across diverse populations and minimizing barriers to treatment (Chieze et al., 2021).
Community incorporation: The emphasis must be upon shifting towards community-based services from institutional care with a focus on incorporation into compassionate living provision and society.
Minimizing stigma: There is a need to implement public awareness campaigns and policies to overcome discrimination and stigma, reinforcing acceptance along with an analysis.
Comprehensive approach: It becomes important for the service providers to involve ongoing support services, rehabilitation, treatment, early intervention and prevention into the policies (Chieze et al., 2021).
Intersectoral collaboration: It becomes important to build up coordination among education, social welfare, health and other appropriate sectors in order to address the social determinants of mental health
Evidence and data-based practices: The service providers are require to use research and data in order to inform the development of policy and make sure successful implementation of mental health programs (Chieze et al., 2021).
Mental health at work: It is strongly recommended to identify the workplace as a major setting for the purpose of adopting transformative action and promoting health (Jokinen et al., 2021). This involves adopting worker training, manager training along with organizational interventions.
Engaging stakeholders: The service providers must make sure individuals with lived experience of mental health conditions, other stakeholders and family members are engaged into the process of policy-making.
Capacity development: The capacity should be upon investing into capacity and training building of mental health providers along with non-specialist staff in order to improve service delivery.
Incorporation into primary care: It is recommended to incorporate mental health services within primary care to minimize barriers and enhance access (Jokinen et al., 2021).
Telemedicine: The service providers are also required to expand the utilization of telemedicine and digital interventions to enhance access to care.
Conclusion
This portfolio critically reviews HSC policies, ethics and legal frameworks regarding the intersection of health and social care and mental capacity in particular. It focuses on the fact that ethical dilemmas, the systemic confines, and changing laws influence professional decision-making and have an effect on vulnerable groups, such as the elderly. The evolution of mental capacity policies through history has happened within an institutionalization to person-centered planning with a focus on autonomy and human rights. However, legislation has progressed, e.g. Mental Capacity Act 2005, but there have nonetheless been difficulties. There are continuing issues with mental capacity assessments being inadequate, systemic barriers, and ethical tensions between protecting and promoting autonomy.
Furthermore, there are problems of compliance and legal accountability regarding safeguards such as the Deprivation of Liberty Safeguards (DoLS). This gap needs to be filled with a more integrated and proactive approach. This includes advancing mental capacity assessments interprofessionally, improving awareness of advance care planning, and improving the statutory frameworks for consistency. Yet, healthcare professionals have to become trained to understand the complexity of the decisions they have to make to ensure the policies become useful protections.
HSC must be able to ensure that obligations imposed by precedent enmesh themselves with the ethical imperatives of protecting vulnerable populations in the legal system that protects and serves them. To ensure just and equitable healthcare, continuous policy refinement, reinforced regulatory oversight, and an ethical practice will be a priority. The solution addresses systemic flaws in a way that can help promote ethical responsibility and therefore create a more inclusive, effective and compassionate healthcare system that puts the rights and dignity of individuals to the forefront of care delivery.
It has been analyzed that evaluating and admiring mental capacity presents multifaceted ethical dilemmas within HSC since it requires harmonizing autonomy with the requirement for protection. However, there is a need to implement public awareness campaigns and policies to overcome discrimination and stigma, reinforcing acceptance along with an analysis.
Students across disciplines often struggle with tight deadlines, complex topics, and academic pressure. Native Assignment Help delivers reliable online assignment help with expert writers, clear structure, proper referencing, and quality content that helps students succeed with confidence.
References
- Bifarin, O., & Stonehouse, D. (2021). Autonomy and capacity: the ethical and legal considerations. British Journal of Healthcare Assistants, 15(11), 545-549.https://researchonline.ljmu.ac.uk/id/eprint/17121/8/Autonomy%20and%20Capacity%20The%20Ethical%20and%20Legal%20Considerations.pdf
- Care Quality Commission. (2025). Regulating health and social care services. Retrieved fromhttps://www.cqc.org.uk/
- Caringforcare.co.uk. (2024, December 11). An In-depth Look at the History of the Mental Capacity Act. Caring for Care.https://caringforcare.co.uk/mental-capacity-act-history/
- Chieze, M., Clavien, C., Kaiser, S., & Hurst, S. (2021). Coercive measures in psychiatry: a review of ethical arguments. Frontiers in psychiatry, 12, 790886. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.790886/pdf
- Gan, J.M., Riley, J., Basting, R., Demeyere, N. and Pendlebury, S.T., 2023. Decision-making capacity in older medical in-patients: frequency of assessment and rates of incapacity by decision-type and underlying brain/mind impairment. Age and Ageing, 52(9), p.afad171.https://academic.oup.com/ageing/article-pdf/52/9/afad171/51624497/afad171.pdf
- Gentsch, A. & Kuehn, E., (2022). Clinical manifestations of body memories: The impact of past bodily experiences on mental health. Brain sciences, 12(5), p.594.https://www.mdpi.com/2076-3425/12/5/594
- Health and Care Professions Council. (2025). Standards and guidance for health and care professionals. Retrieved fromhttps://www.hcpc-uk.org/
- Jokinen, A., Stolt, M., & Suhonen, R. (2021). Ethical issues related to eHealth: an integrative review. Nursing ethics, 28(2), 253-271. https://journals.sagepub.com/doi/pdf/10.1177/0969733020945765
- Kirkbride, J. B., Anglin, D. M., Colman, I., Dykxhoorn, J., Jones, P. B., Patalay, P., ... & Griffiths, S. L. (2024). The social determinants of mental health and disorder: evidence, prevention and recommendations. World psychiatry, 23(1), 58-90.https://onlinelibrary.wiley.com/doi/pdf/10.1002/wps.21160
- Koutsouleris, N., Hauser, T. U., Skvortsova, V., & De Choudhury, M. (2022). From promise to practice: towards the realisation of AI-informed mental health care. The Lancet Digital Health, 4(11), e829-e840. https://www.thelancet.com/pdfs/journals/landig/PIIS2589-7500(22)00153-4.pdf
- Lewis, A. C., & Green, R. C. (2021). Polygenic risk scores in the clinic: new perspectives needed on familiar ethical issues. Genome Medicine, 13(1), 14. https://link.springer.com/content/pdf/10.1186/s13073-021-00829-7.pdf
- Lewis, J. (2021). Capturing and promoting the autonomy of capacitous vulnerable adults. Journal of medical ethics, 47(12), e21-e21.https://research.manchester.ac.uk/files/216796199/
- Martinez-Martin, N., Luo, Z., Kaushal, A., Adeli, E., Haque, A., Kelly, S. S., ... & Milstein, A. (2021). Ethical issues in using ambient intelligence in health-care settings. The lancet digital health, 3(2), e115-e123. https://www.thelancet.com/pdfs/journals/landig/PIIS2589-7500(20)30275-2.pdf
- McDaid, D., Park, A. L., Davidson, G., John, A., Knifton, L., McDaid, S., ... & Wilson, N. (2022). The economic case for investing in the prevention of mental health conditions in the UK.https://pure.qub.ac.uk/files/293822086/Mental_Health_Foundation_2022_Investing_in_Prevention_Report.pdf
- National Institute for Health and Care Excellence. (2025). NICE guidelines and quality standards. Retrieved fromhttps://www.nice.org.uk/
- Reynolds 3rd, C.F., Jeste, D.V., Sachdev, P.S. & Blazer, D.G., (2022). Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry, 21(3), pp.336-363.https://onlinelibrary.wiley.com/doi/pdf/10.1002/wps.20996
- Ruck Keene, A., Kane, N. B., Kim, S. Y., & Owen, G. S. (2023). Mental capacity—why look for a paradigm shift?. Medical Law Review, 31(3), 340-357.https://academic.oup.com/medlaw/article-pdf/31/3/340/51208555/fwac052.pdf
- The King's Fund. (2022). The Health And Care Act: Six Key Questions. The King’s Fund. https://www.kingsfund.org.uk/insight-and-analysis/long-reads/health-and-care-act-key-questions
- Wies, B., Landers, C., & Ienca, M. (2021). Digital mental health for young people: a scoping review of ethical promises and challenges. Frontiers in digital health, 3, 697072. https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2021.697072/full
- World. (2023, October 20). Mental health of older adults. Who.int; World Health Organization: WHO. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults?
Go Through the Best and FREE Samples Written by Our Academic Experts!
Native Assignment Help. (2026). Retrieved from:
https://www.nativeassignmenthelp.co.uk/health-social-care-policy-ethics-and-law-assignment-48128
Native Assignment Help, (2026),
https://www.nativeassignmenthelp.co.uk/health-social-care-policy-ethics-and-law-assignment-48128
Native Assignment Help (2026) [Online]. Retrieved from:
https://www.nativeassignmenthelp.co.uk/health-social-care-policy-ethics-and-law-assignment-48128
Native Assignment Help. (Native Assignment Help, 2026)
https://www.nativeassignmenthelp.co.uk/health-social-care-policy-ethics-and-law-assignment-48128
- FreeDownload - 39 TimesData Analytics and Machine Learning Assignment Sample
Data Analytics and Machine Learning Assignment Sample Introduction Game...View or download
- FreeDownload - 39 TimesNursing Evidencing Graduate and Transferable Skills Assignment Sample
Introduction - Transferable Skills in Nursing Evidence-based practice...View or download
- FreeDownload - 42 TimesConstruction Management Practice Report
Construction Management Practice (BUIL-1258) Introduction The following...View or download
- FreeDownload - 41 TimesBTM0FYT Technology and the Future of Tourism in Australia Assignment Sample
Introduction Tourism is considered as one of the major contributor in economy...View or download
- FreeDownload - 39 TimesUnit 503 Wider Professional Practice and Development in Education and Training
Wider Professional Practice and Development in Education and...View or download
- FreeDownload - 41 TimesKARL: Transforming Human-Environment Dynamics Assignment Sample
STRATEGIC PROJECT MANAGEMENT Introduction Strategic Project Management...View or download
-
100% Confidential
Your personal details and order information are kept completely private with our strict confidentiality policy.
-
On-Time Delivery
Receive your assignment exactly within the promised deadline—no delays, ever.
-
Native British Writers
Get your work crafted by highly-skilled native UK writers with strong academic expertise.
-
A+ Quality Assignments
We deliver top-notch, well-researched, and perfectly structured assignments to help you secure the highest grades.



