Medication Administration Assessment Sample
A reflective nursing assignment applying Driscoll’s framework to dementia care, dignity, communication, and skin integrity.
Ph.D. Experts For Best Assistance
Plagiarism Free Content
AI Free Content
Medication Administration For Dementia Patient Using Driscoll's Framework
Introduction
This study will reflect on the aspects of providing care to a patient with dementia with reference to the skill of skin integrity and personal cleanliness. In accordance with the framework that Driscoll identified in 2007, this paper aims to apply the “What?”, “So What?”, and “Now What?” model done at the workplace with the aim of reflecting professional development as well as improving patient care. Reflection should therefore be adopted in health care since it enhances self- awareness, enhances subsequent practice, and accords with professional advance. The patient in this case scenario is a 76-year-old female admitted on a dementia ward. Thus, she will remain anonymous in this piece as the NMC (2018) Code of Conduct prohibits the breach of patient confidentiality. This patient was initially non-compliant for personal care and therefore needed a lot of communication and understanding of his rights. This reflection will focus on the difficulties faced, measures that were taken to promote and maintain the patient's dignity and safety, as well as the significance of collaboration with the physiotherapy department.
What?
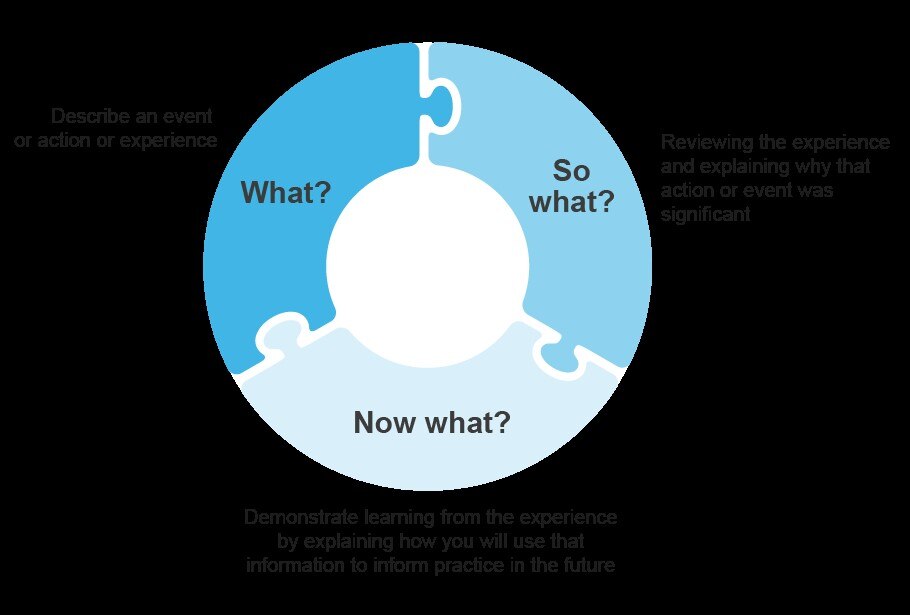
Figure 1: Driscoll’s model of reflection
(Source: https://nshcs.hee.nhs.uk/wp-content/uploads/2023/04/model-of-reflection-v2-1.png)
Situation
In my practical experience, I took care of a 76-year-old female patient or Mrs. X in a dementia unit where she had been admitted the previous night and had not undergone physiotherapy assessment, this meant she could not be moved onto a chair. She was confused and at first they had to restrain her from performing her personal activities such as washing. However, due to lack of communication and the culture of owing her, I managed to motivate her to be more involved in the washing process.
Skills required to be Explored
The two skills I will reflect on include the management of skin integrity and personal patient care of a patient with dementia (Gerlach et al. 2022). Washing of the skin and application of barrier creams is vital in older patients who are in critical situations since they can easily be affected by pressure sores. This skill makes you respect, does not permit infections and improves overall health.
Learning Expectations
Before performing this task, it was my desire to learn how to approach a reluctant patient, address any aggression, and remain professional at the same time as the demonstration. Concerning the care of the patients with dementia, especially those with reduced mobility, I wished to know how skin integrity is crucial (Kim et al. 2021). I discovered that without fear from the patient, this is true because the more I tried to make conversation with the patient and offer her choices such as what she wants to wear, the more cooperative she becomes.
Unexpected observations and barriers
One of the major issues involved the patient’s lack of want of personal care at the initial times which required populism to have her as her consent. Even simple changes in behavior, for instance, describing each step to her and letting her have a little power over her decisions made her more compliant (Scherrer et al. 2021). There was redness and blanching in her groin area so I was able to point out that it is necessary to examine skin changes and apply the corresponding creams to avoid deterioration.
Self-Assessment
In communication, I was able to calm the patient, and gain their cooperation easily. Nevertheless, I had a bit of difficulty in handling the measures of independence and dependence specifically in meeting her hygiene requirements (Appel et al 2021). One staff member added, in a positive feedback section after the procedure, that I was patient and did not tarnish the dignity of any participants. However, I was encouraged to keep building confidence in dealing with resistance outcomes of dementia patients and search for more strategies that would help increase compliance among the patients.
So what?
Effective communication in caring of Dementia
This also involved communication when catering for the needs of a patient with the ailment hence putting into consideration his or her state of health. This patient was non-compliant to bathe, which is a typical issue in the management of the elderly especially those with dementia as they do not understand what is happening to them (Wiemken et al. 2021). Within the interaction, I realized that one had to meet her in a friendly tone, look at her directly and explain things in a simple language that she could understand. The recommendations are that there is a need to also adopt person-centered approaches while communicating with the patients and this involves the use of gestures, avoiding the use of complicated words or languages, and it is also important to ensure that the environment of the patient is calm. I followed these recommendations, where I kept on calming the patient down and avoiding pressuring him by hurrying him up (Juneja et al. 2021). I could also improve my communication skills on the given patient by using validation therapy strategies for example, expressing an understanding of her feelings and then changing the focus to a less resistive subject. I can also enhance my approach towards resolving similar matters in the course of subsequent practice by using the expressed methods.
Maintenance of patient dignity
Self-fulfillment and patients’ rights are also significant components of personal care where the evaluation should be made for violation of the patient’s rights or disrespect of his/her dignity. This patient did not want to participate in washing and forcing care upon her would be against the NM C’s code of conduct and ethical regulation (NMC 2018). To avoid putting pressure on her to give me consent, I kept escorting her gently until all her clothes were off but with an emphasis of closing curtains to avoid either her being exposed or losing heat due to cold draught. This paper will focus on the role of dignity in care especially for the patients with dementia since this domain is a core value when nursing patients (Ruangritchankul et al. 2021). Studies carried out by various authors indicate that patient dignity requires choices to be made on their behalf, good body postures and inviting the patient to participate in arriving at certain decisions. In this case, my actions were by these principles by respecting her need for comfort and giving her some ability to manage her personal hygiene (Xing et al 2025). In future practice, it would also be useful to attempt to reminisce more frequently with her by talking to her about past activities and she may respond positively and willingly when fewer incentives are offered.
Pressure Area care and Skin integrity
An interrelated aspect of personal care is skin health and assessment in the elderly that is at a higher risk of developing pressure ulcers because they embrace restricted movements and fragile skin (NICE, 2021). When washing, I observed erythema and blanching in the groin region on the patient’s body which are risk factors of skin breakdown (Zhang et al. 2022). I used an appropriate barrier cream in an effort to minimize formation of pressure ulcers and I reported the same to the senior nurse for further supervision. From the EPUAP (2019) perspective, it is crucial to prevent pressure injuries from occurring and evaluation of the skin is essential where formal needs to be performed every day. I followed the guidelines that I have to assess the patient's skin for signs of breakdown and intervene to prevent its occurrence. I understand that it is necessary to refresh the best practices for repositioning and pressure relief in clients who are not assessed by a physiotherapist yet (Appel et al. 2021). I will be able to prevent the risk factors and intervene more effectively if I come up with a better understanding of both of them.
Role of Physiotherapy
The final aspect that made a strong impact from this experience was the interprofessional relations, particularly, mobility and physiotherapy. As indicated in this case, Mrs. X was only admitted the previous night and hence, her status on mobility had not been ascertained through a physiotherapy assessment. This restricted the possibility to reposition her into a chair as is an important factor which should be taken into consideration when performing personal nursing interventions (Scharre et al. 2021). The mobility status of a patient is significant in the evaluation process of a physiotherapy plan and to reduce the chances of a fall or worsened health condition. The literature indicates that early and timely mobility evaluations can be risky because it decreases muscle strength and development of pressure ulcers. Thus, not only did I stay true to the procedure by not moving the patient without an assessment on her condition, but I also realized the need to encourage earlier requests for physiotherapy as a way to prevent possible health complications of immobility. Hence, in the future practice, it will be advisable for me to report such cases early and involve physiotherapists to consider appropriate actions as early as possible. This experience emphasized the importance of communication, patient’s dignity, and management of the skin integrity, as well as teamwork with other members of the team in management of patients with dementia. In the light of the above formulation based on Driscoll’s model, some aspects that have highlighted practice strength include showing courtesy and keeping the patient informed with dignity (Shu and Woo, 2021). Nevertheless, there is communication, working with patients, their families, and nurses, validation therapy, pressure area care, pressure ulcer prevention and early involvement of physiotherapy professionals, where I have realized areas where personal development is needed.
Now what?

Figure 2: The Care Tips of Dementia
(Source: https://www.homage.sg/wp-content/uploads/2020/04/Dementia-Care-Tips-700x474.png)
Enhancement of Communication Technologies
Since learning about communication tools that have to be used aurally and orally while caring for patients with dementia, I shall enhance the use of certain approaches that will ensure that I engage the patients adequately (Scherrer et al. 2021). Next time, I will apply the validation therapy more actively, that is repeating the patient’s emotion and calming him down in order to redirect his attention. I will also use other forms of body language by mirroring some of the actions and facial expressions of these patients as a way of proving understanding and promoting some level of confidence in themselves (Sun et al. 2023). These methods can be used to increase patients’ involvement with healthcare providers and enhance attitudes of cooperation and general health.
Strengthening of the patient centered care
To improve the future practice of enhancing dignity in care, therefore, I will increase patient’s independence through choice in the care they receive by involving them in decision-making processes pertaining to their care. For instance, I will use certain questions such as, “Do you wish to rinse out your face or hands first?” Thus, such questions can be specific rather than general in cases that may lead to confusion. I will make it calmer and more comfortable to reduce discomfort especially when helping the patient with his or her needs (Jonsdottir, and Gunnarsson, 2021). These changes are compatible with the recommendations set in relation to the promotion of dignity in care and will improve the patient’s satisfaction with the service as they will feel valued.
Improvement of knowledge about care of pressure area
To enhance my practice in maintaining skin integrity, I will expand my knowledge regarding the pressure ulcer prevention together with the present NICE guidelines to take additional training and any available skin assessment and care courses (NICE, 2021). I will also ensure that I adopt early intervention strategies by being more effective in trying to notice any form of risk as well as ensuring that I report any observed risk promptly (Murroni et al. 2021). Thus, I will be improving patients’ condition and decreasing the risks for further complications such as infections or pressure sore formation with subsequent discomfort.
Assessments for early physiotherapy
Since the first few days it an effective attempt in mobilizing oneself should be made I shall start insisting on ordering immediate physiotherapy tests. In the future practice, I will report delays such as those in mobility assessments more aggressively to ensure that the patients get required interventions as early as possible to prevent negative impacts to their functions (Weidmann et al. 2025). Since being around the physiotherapists I’ve come to understand that liaising with them would assist me in providing an integrated approach to the patients.
Development of the plan
To achieve these changes, I will consult with other staff members in order to get advice on how they communicate within the working environment (Zhang et al. 2022). I will also continue to read more and learn how to fight for dignity in care and easy prevention of pressure ulcers for the patients in addition to gaining more knowledge in advocacy for combined efforts from other professionals in order to enhance the outcomes of patients with dementia.
Conclusion
Relating this experience to the concepts learned from Driscoll’s model has enhanced my knowledge on communication, patient centered care, skin care and assessment of the physical therapy before the patient undergoes a procedure on their abdomen. From this process, I can find out the weak aspects that need to be worked upon in the future like communication, proper implementation of timely interventions to remain intact and exploring more about pressure ulcer prevention. The multiple reflections made have helped me to enhance the level of care: attentive and informed. In future practice, I shall incorporate these findings in order to enhance the improvement of the patients’ status, minimize the infringement on their dignity and guarantee their safety and comfort. These five artifacts will help in future improvement of my reflection, professionalism and better understanding of the patients’ needs.
Finding reflective nursing assignments challenging? This sample shows how to apply Driscoll’s framework effectively, but every reflection needs a personal, well-structured approach. Our assignment help experts support nursing students with reflective writing, evidence-based practice, and proper academic referencing—helping you submit confident, high-quality work on time.
Reference List
Journals
Appel, L., Kisonas, E., Appel, E., Klein, J., Bartlett, D., Rosenberg, J. and Smith, C.N., 2021. Administering virtual reality therapy to manage behavioral and psychological symptoms in patients with dementia admitted to an acute care hospital: results of a pilot study. JMIR formative research, 5(2), p.e22406.
Dresden, S.M., Taylor, Z., Serina, P., Kennedy, M., Wescott, A.B., Hogan, T., Shah, M.N., Hwang, U., Aggarawal, N.T., Allore, H. and Aloysi, A., 2022. Optimal emergency department care practices for persons living with dementia: a scoping review. Journal of the American Medical Directors Association, 23(8), pp.1314-e1.
Gerlach, L.B., Maust, D.T., Kales, H.C., Chang, M., Kim, H.M., Wiechers, I.R. and Zivin, K., 2022. Evaluation of antipsychotic reduction efforts in patients with dementia in veterans health administration nursing homes. American Journal of Psychiatry, 179(8), pp.544-552.
Jonsdottir, T. and Gunnarsson, E.C., 2021. Understanding nurses’ knowledge and attitudes toward pain assessment in dementia: a literature review. Pain Management Nursing, 22(3), pp.281-292.
Juneja, S., Dhiman, G., Kautish, S., Viriyasitavat, W. and Yadav, K., 2021. A perspective roadmap for IoMT‐based early detection and care of the neural disorder, dementia. Journal of Healthcare Engineering, 2021(1), p.6712424.
Kim, H.J., Cho, K.R., Jang, H., Lee, N.K., Jung, Y.H., Kim, J.P., Lee, J.I., Chang, J.W., Park, S., Kim, S.T. and Moon, S.W., 2021. Intracerebroventricular injection of human umbilical cord blood mesenchymal stem cells in patients with Alzheimer’s disease dementia: a phase I clinical trial. Alzheimer's Research & Therapy, 13, pp.1-11.
Murroni, V., Cavalli, R., Basso, A., Borella, E., Meneghetti, C., Melendugno, A. and Pazzaglia, F., 2021. Effectiveness of therapeutic gardens for people with dementia: A systematic review. International journal of environmental research and public health, 18(18), p.9595.
Ruangritchankul, S., Chantharit, P., Srisuma, S. and Gray, L.C., 2021. Adverse drug reactions of acetylcholinesterase inhibitors in older people living with dementia: A comprehensive literature review. Therapeutics and clinical risk management, pp.927-949.
Scharre, D.W., Chang, S.I., Nagaraja, H.N., Wheeler, N.C. and Kataki, M., 2021. Self-Administered Gerocognitive Examination: longitudinal cohort testing for the early detection of dementia conversion. Alzheimer's research & therapy, 13, pp.1-11.
Scherrer, J.F., Salas, J., Wiemken, T.L., Hoft, D.F., Jacobs, C. and Morley, J.E., 2021. Impact of herpes zoster vaccination on incident dementia: a retrospective study in two patient cohorts. PLoS One, 16(11), p.e0257405.
Shu, S. and Woo, B.K., 2021. Use of technology and social media in dementia care: Current and future directions. World journal of psychiatry, 11(4), p.109.
Sun, M., Chen, W.M., Wu, S.Y. and Zhang, J., 2023. Dementia risk after major elective surgery based on the route of anaesthesia: A propensity score-matched population-based cohort study. EClinicalMedicine, 55.
Weidmann, A.E., Proppé, G.B., Matthíasdóttir, R., Tadić, I., Gunnarsson, P.S. and Jónsdóttir, F., 2025. Medication-induced causes of delirium in patients with and without dementia: a systematic review of published neurology guidelines. International Journal of Clinical Pharmacy, pp.1-18.
Wiemken, T.L., Salas, J., Hoft, D.F., Jacobs, C., Morley, J.E. and Scherrer, J.F., 2021. Dementia risk following influenza vaccination in a large veteran cohort. Vaccine, 39(39), pp.5524-5531.
Xing, Y., Pratama, D.P., Wang, Y., Zhang, Y. and Chapman, B.E., 2025. Utilizing Sequential Information of General Lab-test Results and Diagnoses History for Differential Diagnosis of Dementia. arXiv preprint arXiv:2502.15317.
Zhang, Y.R., Wang, J.J., Chen, S.F., Wang, H.F., Li, Y.Z., Ou, Y.N., Huang, S.Y., Chen, S.D., Cheng, W., Feng, J.F. and Dong, Q., 2022. Peripheral immunity is associated with the risk of incident dementia. Molecular Psychiatry, 27(4), pp.1956-1962.
Go Through the Best and FREE Samples Written by Our Academic Experts!
Native Assignment Help. (2026). Retrieved from:
https://www.nativeassignmenthelp.co.uk/medication-administration-assessment-sample-47366
Native Assignment Help, (2026),
https://www.nativeassignmenthelp.co.uk/medication-administration-assessment-sample-47366
Native Assignment Help (2026) [Online]. Retrieved from:
https://www.nativeassignmenthelp.co.uk/medication-administration-assessment-sample-47366
Native Assignment Help. (Native Assignment Help, 2026)
https://www.nativeassignmenthelp.co.uk/medication-administration-assessment-sample-47366
- FreeDownload - 38 TimesEmotional Intelligence in Motivating Assignment
Evaluating The Role Of Emotional Intelligence In Motivating Multicultural...View or download
- FreeDownload - 42 TimesManaging Food and Beverage Operations Assignment Sample
Managing Food and Beverage Operations Assignment...View or download
- FreeDownload - 41 TimesEthical and legal decision making in the context of nursing Assignment Help UK Sample
ETHICAL AND LEGAL DECISION-MAKING IN THE CONTEXT OF NURSING Assignment...View or download
- FreeDownload - 42 TimesFinancial Analysis Of Mark & Spencer Case Study
Financial Analysis Of Mark & Spencer Introduction - Financial...View or download
- FreeDownload - 45 TimesENEB com NLP Assignment Sample
ENEB com NLP 1. Choice of subject/topic In my last NLP assignment, I decided...View or download
- FreeDownload - 0 TimesProfessionalism in the Workplace Assignment Sample
-
100% Confidential
Your personal details and order information are kept completely private with our strict confidentiality policy.
-
On-Time Delivery
Receive your assignment exactly within the promised deadline—no delays, ever.
-
Native British Writers
Get your work crafted by highly-skilled native UK writers with strong academic expertise.
-
A+ Quality Assignments
We deliver top-notch, well-researched, and perfectly structured assignments to help you secure the highest grades.



